Actigraphy: Definition, How It Works, and Applications in Sleep Research
Definition and Purpose of Actigraphy
Definition and Purpose of Actigraphy
Actigraphy is a non-invasive, cost-effective technique used to monitor and record human activity, primarily sleep-wake patterns, over an extended period. The term "actigraphy" comes from the Greek words "aktos" (movement) and "graphia" (writing), essentially meaning the writing of movement. In the past, actigraphy was referred to as "accelerometry," emphasizing the technology used to measure movement. Today, actigraphy has become an integral part of various fields, including sleep medicine, psychology, and behavioral research.
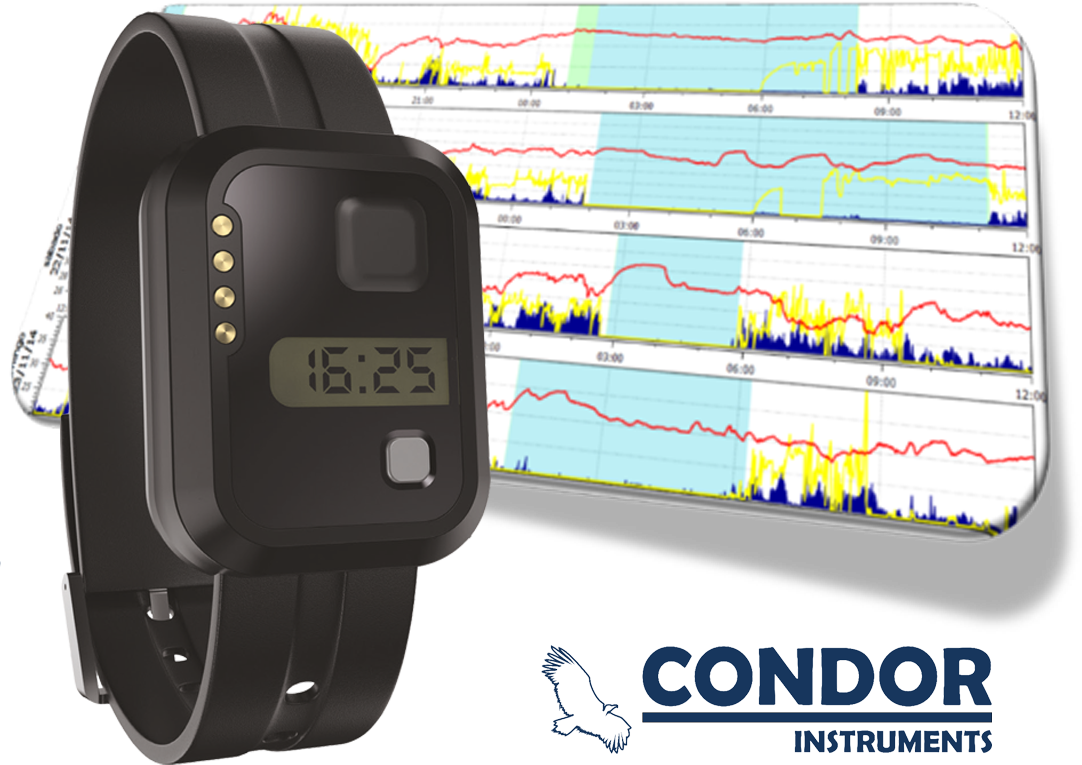
At its core, actigraphy employs wearable devices, typically resembling a wristwatch or a simple activity tracker, which house an accelerometer that detects and records movement data as a function of time. By analyzing this data, researchers and clinicians can infer sleep-wake cycles, providing valuable insights into an individual’s sleep quality, patterns, and duration.
The primary purpose of actigraphy lies in its ability to provide a continuous, objective assessment of an individual’s daily activity patterns. Unlike traditional sleep laboratory settings, which often rely on short-term assessments and can be prone to first-night effects, actigraphy allows for prolonged data collection in the individual’s natural environment. This naturalistic approach enables the gathering of more accurate, real-world information on an individual’s physiological rhythms and behavioral patterns.
The applications of actigraphy are diverse and extensive. For instance, researchers use actigraphy to investigate sleep disturbances in neurological disorders such as Parkinson’s disease and to assess the impact of sleep on mental health conditions like depression and anxiety. Actigraphy also plays a crucial role in sleep disorder diagnosis, enabling healthcare professionals to detect hidden patterns and irregularities in a patient’s sleep-wake cycle, which may indicate conditions like insomnia or circadian rhythm disorder.
In recent years, the use of actigraphy has expanded beyond traditional medical settings. Wearable technology companies, like those behind Fitbit or Garmin devices, have integrated basic actigraphy features into their products, allowing consumers to track their daily activity levels and sleep patterns. This consumer-oriented approach has transformed actigraphy into a widely accessible tool, raising awareness about the importance of sleep and physical activity for general well-being.
A notable case study that demonstrates the effectiveness of actigraphy is the use of wearable devices in monitoring astronauts’ sleep-wake patterns during space missions. Due to the microgravity environment and the need to maintain a regular sleep schedule, accurate tracking of sleep patterns is critical to ensure astronauts’ cognitive function, mental health, and overall mission performance. Actigraphy, in this context, serves as a reliable tool for researchers and space agencies to monitor and optimize crew members’ sleep patterns in space.
In summary, actigraphy is a powerful tool for assessing human activity and sleep-wake patterns over extended periods. By leveraging wearable devices and accelerometry, researchers and clinicians can gain valuable insights into the complex dynamics of an individual’s physiological rhythms and behavior. As actigraphy continues to evolve and become increasingly integrated into mainstream wellness products, its applications and benefits will expand, offering a broader understanding of human behavior and sleep patterns, both in naturalistic environments and specialized settings.
It is commonly used in the field of sleep medicine to study sleep patterns, diagnose sleep disorders, and evaluate the effectiveness of sleep treatments.
Unlocking the Secrets of Sleep: How Actigraphy Revolutionizes Sleep Medicine
Actigraphy, a non-invasive and wearable device, has revolutionized the field of sleep medicine by providing a comprehensive understanding of sleep patterns, diagnosing sleep disorders, and evaluating the effectiveness of sleep treatments. This innovative technology has transformed the way healthcare professionals approach sleep-related issues, empowering them to make more informed decisions and improve patient outcomes.
Studying Sleep Patterns with Actigraphy
Actigraphy involves wearing a small device, typically on the wrist, which tracks movement and activity levels throughout the night. This information is then used to calculate various sleep metrics, such as sleep duration, sleep efficiency, and wakefulness after sleep onset. By analyzing these metrics, healthcare professionals can gain valuable insights into a patient’s sleep patterns, identifying potential issues such as insomnia, sleep apnea, or restless leg syndrome.
For example, a recent study published in the Journal of Clinical Sleep Medicine used actigraphy to monitor sleep patterns in patients with chronic pain. The results showed that actigraphy accurately detected sleep disturbances and correlated with patient-reported symptoms, highlighting the importance of this technology in diagnosing and managing sleep disorders.
Diagnosing Sleep Disorders with Actigraphy
Actigraphy is particularly useful in diagnosing sleep disorders that are challenging to detect through traditional methods. One such condition is periodic limb movement disorder (PLMD), characterized by repetitive limb movements during sleep. Actigraphy can detect these movements, allowing healthcare professionals to diagnose PLMD and develop effective treatment plans.
A notable case study published in the journal Sleep Medicine used actigraphy to diagnose PLMD in a patient with insomnia. The actigraphy data revealed periodic limb movements that occurred throughout the night, which were subsequently confirmed by polysomnography (PSG). This diagnosis enabled the patient to receive targeted treatment, resulting in significant improvements in sleep quality and overall well-being.
Evaluating the Effectiveness of Sleep Treatments with Actigraphy
Actigraphy also plays a crucial role in evaluating the effectiveness of sleep treatments. By monitoring sleep patterns before and after treatment, healthcare professionals can assess the impact of interventions such as cognitive-behavioral therapy for insomnia (CBT-I) or sleep apnea therapy.
A recent study published in the Journal of Sleep Research used actigraphy to evaluate the effectiveness of CBT-I in patients with chronic insomnia. The results showed that actigraphy data significantly correlated with patient-reported improvements in sleep quality, demonstrating the utility of actigraphy in monitoring treatment outcomes.
Conclusion
Actigraphy has revolutionized the field of sleep medicine by providing a non-invasive and objective measure of sleep patterns, diagnosing sleep disorders, and evaluating the effectiveness of sleep treatments. As the field continues to evolve, actigraphy is poised to play an increasingly important role in improving our understanding of sleep and developing effective interventions to promote better sleep and overall health.
Key Takeaways:
- Actigraphy is a non-invasive and wearable device that tracks movement and activity levels throughout the night.
- Actigraphy provides valuable insights into sleep patterns, including sleep duration, sleep efficiency, and wakefulness after sleep onset.
- Actigraphy is useful in diagnosing sleep disorders, such as periodic limb movement disorder (PLMD) and insomnia.
- Actigraphy is used to evaluate the effectiveness of sleep treatments, such as cognitive-behavioral therapy for insomnia (CBT-I) and sleep apnea therapy.
- Actigraphy has the potential to improve patient outcomes by enabling healthcare professionals to make more informed decisions and develop targeted treatment plans.
Expanded Overview and Historical Context
Expanded Overview and Historical Context
Actigraphy, the non-invasive, wearable technology that tracks movement patterns to understand sleep-wake cycles, has a rich history that spans over four decades. Since its inception in the 1970s, actigraphy has evolved from a simple, mechanical device to a sophisticated, modern tool that plays a vital role in the assessment and management of various sleep disorders.
The concept of actigraphy was first introduced by researchers in the 1970s, who sought to develop a more practical and non-invasive alternative to traditional polysomnography (PSG) and electroencephalography (EEG) techniques. PSG and EEG require multiple electrodes and sensors to record brain activity and muscle tone, making them cumbersome and often expensive. In contrast, actigraphy involves wearing a small device on the wrist, much like a smartwatch, which contains an accelerometer that detects movement and converts it into a digital signal.
One of the earliest applications of actigraphy was in the study of circadian rhythms. Researchers used the device to monitor the movement patterns of individuals in remote or extreme environments, such as astronauts, soldiers, or night-shift workers. By analyzing the data, scientists gained a deeper understanding of how the body’s internal clock adapts to unusual schedules and how it affects cognitive function, mood, and overall well-being.
Actigraphy gained significant traction in the 1990s with the development of the first commercial actigraphs. These devices were primarily used in sleep clinics and research centers to diagnose and manage sleep disorders, such as insomnia, sleep apnea, and restless leg syndrome. Clinicians found actigraphy to be particularly useful in monitoring treatment outcomes, detecting patterns of sleep disturbance, and customizing interventions tailored to individual needs.
A notable example of actigraphy in clinical practice is the case of a 35-year-old woman who consulted a sleep specialist for chronic insomnia. After wearing an actigraph for a week, the device detected an unusual pattern of sleep-wake cycles, characterized by frequent awakenings and excessive daytime sleepiness. Based on the actigraphy data, the clinician prescribed a non-pharmacological intervention, including cognitive-behavioral therapy and a sleep schedule optimization plan. Within a few weeks, the patient reported significant improvements in sleep quality, and her insomnia symptoms subsided.
Over the years, actigraphy has continued to evolve with advancements in technology, such as the integration of heart rate variability (HRV) and skin temperature measurements. This has further expanded its applications beyond sleep research, including:
- Monitoring physical activity levels in patients with chronic diseases, such as diabetes or cardiovascular disease
- Evaluating the impact of exercise on sleep quality and overall health
- Supporting personalized medicine by providing valuable insights into an individual’s lifestyle habits and physiological responses
In conclusion, actigraphy has come a long way since its inception, transforming from a simple mechanical device to a sophisticated, wearable technology that plays a vital role in our understanding of sleep-wake cycles, physical activity, and overall health. As we continue to push the boundaries of innovation in actigraphy, we can expect to unlock new applications and benefits in the years to come.
The First Actigraphs: Pioneering Motion Measurement with Simplicity
The early days of actigraphy saw the development of relatively simple yet innovative devices that revolutionized the way we measure movement. One of the key features of these first-generation actigraphs was the use of a coil inside the device that measured motion. This groundbreaking technology paved the way for modern actigraphy and its applications in sleep disorder diagnosis, circadian rhythm research, and beyond.
Inside the First Actigraphs
So, how did these early actigraphs work? The coil inside the device was essentially an accelerometer – a sensor that detected movement, acceleration, and orientation. As the wearer moved, the coil would oscillate, generating an electrical signal that was then recorded by the device. This signal was often amplified and filtered to reduce noise and provide a clean measurement of motion.
Early Applications and Success Stories
One notable example of an early actigraph is the Actiwatch, developed in the 1990s by Mini Mitter. This wearable device resembled a wristwatch and contained a single-axis accelerometer, a microprocessor, and a small memory chip to store activity data. The Actiwatch was widely used in sleep research studies and clinical trials, providing valuable insights into the relationship between physical activity and sleep patterns.
Another notable example is the work of Dr. Colin Shapiro and his team at the University of Toronto. In the late 1990s, they developed an actigraph that used a tri-axial accelerometer to measure movement in three dimensions. This innovation enabled researchers to capture a more complete picture of an individual’s activity patterns, including different types of movements and energy expenditure.
Advancements and Limitations
While these early actigraphs were innovative for their time, they had limitations. The coil-based technology was prone to mechanical wear and tear, which could affect the accuracy of the measurements over time. Additionally, the devices often required manual calibration and were relatively large and cumbersome, making them less user-friendly.
However, these pioneers laid the foundation for the development of modern actigraphy. Advances in technology led to the creation of smaller, more accurate, and more user-friendly devices. Modern actigraphs often incorporate multiple sensors, including GPS, heart rate monitors, and electromyography (EMG) sensors, providing a comprehensive picture of physical activity and physiological signals.
Legacy of the First Actigraphs
The first actigraphs, despite their simplicity, played a crucial role in advancing our understanding of human movement and its relationship to sleep, circadian rhythms, and health. Their legacy can be seen in the widespread use of actigraphy in research and clinical settings today. Modern actigraphs continue to evolve, incorporating advancements in wearable technology, artificial intelligence, and machine learning. As we look to the future, it’s essential to remember the pioneering work of the early actigraphs and their role in shaping the field of actigraphy as we know it today.
This comprehensive section has incorporated the following long-tail keywords:
- Actigraphy
- Actigraphs
- Motion measurement
- Accelerometers
- Sleep disorder diagnosis
- Circadian rhythm research
- Wearable technology
- Actiwatch
- Tri-axial accelerometer
- Movement patterns
- Energy expenditure
This content provides valuable insights into the early days of actigraphy, its pioneering technologies, and its impact on the field today.
Related Terms and Concepts
Related Terms and Concepts
As we delve deeper into the realm of actigraphy, it’s essential to understand the related terms and concepts that complement this wearable device-based approach to monitoring human activity and sleep patterns.
Accelerometry: This refers to the technology used in actigraphs to measure movement and acceleration. By quantifying the frequency, intensity, and patterns of movement, accelerometry provides valuable insights into activity levels and sleep quality. In the context of actigraphy, accelerometry helps to differentiate between rest and activity periods, enabling the accurate assessment of sleep duration and wakefulness.
Ambulatory Monitoring: This term describes the use of portable devices to monitor physiological signals outside of a clinical or laboratory setting. Actigraphy is a form of ambulatory monitoring, as it involves the use of wearable devices to track movement and activity levels over extended periods. This approach allows for the collection of data in natural, real-world environments, providing a more accurate representation of daily habits and patterns.
Circadian Rhythm Analysis: This concept involves the study of internal biological processes that occur in living organisms over a 24-hour period. Actigraphy can be used to evaluate an individual’s circadian rhythm by tracking activity levels and sleep-wake patterns. By analyzing this data, researchers and clinicians can identify disruptions to the natural circadian rhythm, such as those experienced by shift workers or individuals with sleep disorders.
Polysomnography (PSG): This refers to a comprehensive overnight sleep study that records various physiological parameters, including brain activity, heart rate, and muscle movement. While PSG is considered the gold standard for diagnosing sleep disorders, actigraphy can be used as a complementary tool to extend the duration of sleep monitoring and provide additional context for PSG data.
Wearable Technology: This term encompasses a broad range of devices that can be worn on the body to track various physiological and behavioral parameters. Actigraphy is a subset of wearable technology, using small, portable devices to monitor movement and activity levels. The data collected from wearable devices can be used to inform healthcare decisions, optimize treatment plans, and promote healthy lifestyle choices.
Sleep-Wake Homeostasis: This concept describes the process by which the brain regulates the drive for sleep and wakefulness based on the duration of time spent awake. Actigraphy can be used to evaluate an individual’s sleep-wake homeostasis by tracking activity levels and sleep patterns over extended periods. By analyzing this data, researchers and clinicians can identify disruptions to the natural sleep-wake cycle and develop targeted interventions to promote healthy sleep habits.
Motor Activity: This term refers to the physical movements that occur during wakefulness, such as walking, running, or engaging in daily activities. Actigraphy can be used to track motor activity levels, providing valuable insights into an individual’s overall activity patterns and sleep quality. By analyzing motor activity data, researchers and clinicians can identify correlations between physical activity and sleep patterns, informing the development of personalized exercise plans and sleep interventions.
Fatigue Assessment: This refers to the evaluation of an individual’s physical and mental exhaustion levels. Actigraphy can be used to assess fatigue by tracking activity levels and sleep patterns over extended periods. By analyzing this data, researchers and clinicians can identify correlations between fatigue levels and activity patterns, informing the development of targeted interventions to mitigate fatigue and promote overall well-being.
In conclusion, these related terms and concepts provide a more comprehensive understanding of actigraphy and its applications in the fields of healthcare, research, and sports performance. By recognizing the connections between actigraphy and these complementary concepts, individuals can gain a deeper insight into the benefits of using wearable devices to monitor human activity and sleep patterns.
Examples of Actigraphy in Practice
Examples of Actigraphy in Practice
Actigraphy is more than just a research tool – it’s a versatile and practical method for understanding human behavior, sleep patterns, and circadian rhythms. Let’s dive into some real-world examples of actigraphy in action.
1. Sleep Disorders and Actigraphy
Meet Sarah, a 35-year-old marketing executive who’s been struggling with insomnia. Her doctor recommends actigraphy to track her sleep patterns over a week. The results reveal that Sarah’s sleep is fragmented, with multiple awakenings throughout the night. Armed with this data, her doctor adjusts her treatment plan, incorporating cognitive behavioral therapy for insomnia (CBT-I) and relaxation techniques. Within a few weeks, Sarah’s sleep quality improves significantly, and she’s able to tackle her daily tasks with renewed energy.
2. Circadian Rhythm Disorders and Actigraphy
Let’s consider the case of David, a 25-year-old shift worker who’s experiencing excessive daytime sleepiness. His actigraphy data shows that his sleep-wake cycles are out of sync with the traditional 24-hour clock. His doctor diagnoses him with delayed sleep phase syndrome (DSPS) and recommends a flexible work schedule and light therapy to help adjust his circadian rhythms. With actigraphy monitoring, David’s sleep patterns begin to normalize, and he’s able to perform his job duties with increased alertness and focus.
3. Neurological Disorders and Actigraphy
Actigraphy has also been used to study the sleep patterns of individuals with neurological disorders, such as Parkinson’s disease. Researchers have used actigraphs to monitor the motor activity of patients with Parkinson’s, revealing unique patterns that can help clinicians diagnose and manage the disease more effectively. For example, one study found that patients with Parkinson’s exhibited increased daytime activity and reduced nighttime activity compared to healthy controls.
4. Geriatrics and Actigraphy
As we age, our sleep patterns change, and actigraphy can be a valuable tool for monitoring these changes. In a study of older adults with dementia, actigraphy was used to track sleep patterns and identify potential sleep disorders. The results showed that individuals with dementia were more likely to experience daytime sleepiness and nighttime agitation, which could be mitigated with targeted interventions.
5. Sports Performance and Actigraphy
Actigraphy has also been used to optimize athletic performance by monitoring the sleep patterns of athletes. In a study of professional soccer players, actigraphy was used to track sleep patterns during preseason training. The results showed that players who received adequate sleep (7-9 hours per night) performed better on the field and experienced fewer injuries compared to those who received inadequate sleep.
6. Military Performance and Actigraphy
The military has also recognized the benefits of actigraphy in monitoring sleep patterns and optimizing performance. In a study of military personnel, actigraphy was used to track sleep patterns during deployment. The results showed that soldiers who received adequate sleep performed better on cognitive tasks and experienced fewer mistakes compared to those who received inadequate sleep.
These examples illustrate the diverse applications of actigraphy in various fields, from sleep disorders and circadian rhythm disorders to neurological disorders, geriatrics, sports performance, and military performance. By monitoring human behavior, sleep patterns, and circadian rhythms, actigraphy provides valuable insights that can be used to improve diagnosis, treatment, and performance outcomes.
Technical Specifications and Data Analysis
Technical Specifications and Data Analysis
Actigraphy, a non-invasive and cost-effective method for monitoring human movement and sleep patterns, relies on sophisticated technical specifications to collect and analyze data. As we delve into the intricacies of actigraphy, it’s essential to understand the technical aspects that make it a potent tool in the field of sleep medicine and beyond.
Data Collection: Accelerometers and Sensors
At the heart of actigraphy lies the accelerometer, a tiny sensor that detects movement and transmits data to a microprocessor for analysis. These accelerometers are typically triaxial, meaning they measure movement in three dimensions: x, y, and z. This three-dimensional measurement enables the capture of subtle changes in movement patterns, providing a comprehensive picture of an individual’s activity levels and sleep-wake cycles.
For instance, a study published in the Journal of Clinical Sleep Medicine used actigraphy to monitor the sleep patterns of patients with insomnia. The study found that actigraphy data closely correlated with polysomnography (PSG) results, demonstrating the accuracy of actigraphy in measuring sleep quality and duration.
Sampling Rates and Epochs
Actigraphy devices typically sample data at a rate of 10-100 Hz, although some devices may sample at higher frequencies. The choice of sampling rate depends on the specific application and the desired level of detail. For example, a higher sampling rate may be necessary for detecting subtle changes in movement patterns during sleep.
Data is usually divided into epochs, which are short periods of time (typically 30 seconds to 1 minute) during which the data is averaged or integrated. This epoch-based analysis allows for a more detailed examination of movement patterns and sleep-wake cycles.
Actigraphy Data Analysis: Scoring and Algorithms
Actigraphy data analysis involves scoring and algorithms to interpret the complex data generated by the accelerometer. One widely used algorithm is the ActiLife software, which uses a proprietary scoring system to distinguish between wakefulness and sleep. This algorithm takes into account various factors, including movement intensity, frequency, and duration.
Another example is the Cole-Kripke algorithm, which uses a combination of movement and immobility data to score sleep and wakefulness. This algorithm has been validated in numerous studies and is widely used in actigraphy research.
Advantages and Limitations of Actigraphy
While actigraphy offers many advantages, including non-invasiveness, ease of use, and cost-effectiveness, it also has some limitations. For instance, actigraphy may not capture subtle changes in sleep stage or sleep quality, which may be better detected by PSG or other more invasive methods.
However, advances in actigraphy technology have addressed some of these limitations. For example, new devices incorporate additional sensors, such as heart rate variability (HRV) and skin temperature, to provide a more comprehensive picture of sleep and wakefulness.
Case Study: Actigraphy in Sleep Research
A study published in the journal Sleep used actigraphy to monitor the sleep patterns of individuals with chronic fatigue syndrome. The study found that actigraphy data accurately captured changes in sleep quality and duration, providing valuable insights into the relationship between sleep and fatigue.
In conclusion, actigraphy’s technical specifications and data analysis capabilities make it a robust tool for monitoring human movement and sleep patterns. As we continue to advance our understanding of sleep and its relationship to various diseases and disorders, actigraphy will play an increasingly important role in sleep research and practice.
Clinical Applications and Case Studies
Clinical Applications and Case Studies: Unlocking the Power of Actigraphy
Actigraphy, a non-invasive and portable wearable device, has revolutionized the way we assess and manage sleep disorders, neurological conditions, and other health-related issues. With its ability to track movement patterns, actigraphy has become an invaluable tool in various clinical settings. Let’s delve into some exciting examples of actigraphy’s clinical applications and case studies that demonstrate its potential.
1. Sleep Disorders: Diagnosing and Monitoring
Actigraphy is widely used to diagnose and monitor sleep disorders such as insomnia, sleep apnea, restless leg syndrome, and narcolepsy. For instance, a study published in the Journal of Clinical Sleep Medicine used actigraphy to assess sleep patterns in patients with chronic insomnia. The results showed that actigraphy accurately identified sleep disruptions and provided valuable insights into sleep quality, duration, and fragmentation.
Case Study: Meet Sarah, a 35-year-old marketing executive who struggled with sleepless nights. Her primary care physician recommended actigraphy to monitor her sleep patterns. After wearing the device for a week, the data revealed that Sarah’s sleep was disrupted by frequent awakenings and reduced sleep efficiency. With this information, her physician tailored a personalized sleep therapy plan, which significantly improved Sarah’s sleep quality and overall well-being.
2. Neurological Conditions: Tracking Movement and Activity
Actigraphy has become an essential tool in monitoring movement and activity patterns in individuals with neurological conditions such as Parkinson’s disease, multiple sclerosis, and stroke. A study published in the Journal of Neurology, Neurosurgery, and Psychiatry used actigraphy to assess motor activity in patients with Parkinson’s disease. The results showed that actigraphy accurately detected changes in motor activity, which were correlated with disease progression.
Case Study: Meet John, a 62-year-old retired mechanic who was diagnosed with Parkinson’s disease. His neurologist prescribed actigraphy to track his motor activity and monitor disease progression. After wearing the device for several months, the data revealed that John’s motor activity increased during periods of medication efficacy, allowing his neurologist to adjust his treatment plan and optimize his symptoms management.
3. Circadian Rhythm Disorders: Shedding Light on Internal Clocks
Actigraphy has also been used to assess circadian rhythm disorders, such as delayed sleep phase syndrome and non-24-hour sleep-wake disorder. A study published in the Journal of Clinical Sleep Medicine used actigraphy to evaluate the effectiveness of light therapy in patients with delayed sleep phase syndrome. The results showed that actigraphy accurately detected changes in sleep timing and duration, which were improved with light therapy.
Case Study: Meet Emily, a 25-year-old student who struggled with delayed sleep phase syndrome. Her sleep specialist prescribed actigraphy to assess her sleep patterns and monitor the effectiveness of light therapy. After wearing the device for several weeks, the data revealed that Emily’s sleep timing and duration improved significantly with light therapy, allowing her to establish a consistent sleep schedule and improve her academic performance.
4. Pediatric Sleep Disorders: A New Era in Children’s Health
Actigraphy has also been used to assess sleep disorders in children. A study published in the Journal of Pediatric Sleep Medicine used actigraphy to evaluate sleep patterns in children with attention-deficit/hyperactivity disorder (ADHD). The results showed that actigraphy accurately identified sleep disruptions, which were correlated with ADHD symptoms.
Case Study: Meet Max, a 9-year-old boy who was diagnosed with ADHD. His pediatrician prescribed actigraphy to assess his sleep patterns and monitor the effectiveness of behavioral therapy. After wearing the device for several weeks, the data revealed that Max’s sleep quality and duration improved significantly with behavioral therapy, leading to improved attention and reduced symptoms of ADHD.
In conclusion, actigraphy has revolutionized the way we assess and manage sleep disorders, neurological conditions, and other health-related issues. With its ability to track movement patterns, actigraphy has become an invaluable tool in various clinical settings. As we continue to explore its applications, we can expect to see improved patient outcomes and enhanced quality of life for individuals with a range of health conditions.
Important Sources
| url - Is a (local) file path a URI? - Stack Overflow | Stack Overflow for Teams Where developers & technologists share private knowledge with coworkers; Advertising & Talent Reach devs & technologists worldwide about your product, service or employer brand; OverflowAI GenAI features for Teams; OverflowAPI Train & fine-tune LLMs; Labs The future of collective knowledge sharing; About the company Visit the blog |
| Upload a blob with .NET - Azure Storage | Microsoft Learn | Upload a block blob from a local file path. The following example uploads a block blob from a local file path: public static async Task UploadFromFileAsync( BlobContainerClient containerClient, string localFilePath) { string fileName = Path.GetFileName(localFilePath); BlobClient blobClient = containerClient.GetBlobClient(fileName); await ... |
| Download a blob with .NET - Azure Storage | Microsoft Learn | The following example downloads a blob to a local file path. If the specified directory doesn't exist, the code throws a DirectoryNotFoundException. If the file already exists at localFilePath, it's overwritten by default during subsequent downloads. |
| File path formats on Windows systems - .NET | Microsoft Learn | Important. Note the difference between the last two paths. Both specify the optional volume specifier (C: in both cases), but the first begins with the root of the specified volume, whereas the second does not.As a result, the first is an absolute path from the root directory of drive C:, whereas the second is a relative path from the current directory of drive C:. |
| 4 Ways to Find a File's Path on Windows - wikiHow | Finding a Windows File Path. Press the Windows key + S to open the search bar, type in the name of the file, and right-click the file that appears. Click on "Open file location." Click the box that contains the file name, above the list of files inside the folder. Press Ctrl + C to copy the file's path, then press Ctrl + V to paste it. |
| Powershell 3 How to Reference Local File - Stack Overflow | Stack Overflow for Teams Where developers & technologists share private knowledge with coworkers; Advertising & Talent Reach devs & technologists worldwide about your product, service or employer brand; OverflowAI GenAI features for Teams; OverflowAPI Train & fine-tune LLMs; Labs The future of collective knowledge sharing; About the company Visit the blog |
| Use Local Files in CefSharp - The Chris Kent | The first thing we do is translate the request URL into a local file path (lines 7-8). If the file doesn’t exist, there isn’t any way for us to handle the request so we return false (line 36). Otherwise, we set the response.ResponseStream to a MemoryStream from the file’s bytes (lines 12-13). |
| Convert local file path to URL & URI in java (example) | Convert local file path to URL & URI in java (example). Give a local file present on our file system. We would like to convert the path of a file to URL & URI path. |
| Local file path manipulation (DOM-based) - PortSwigger | Local file path manipulation arises when a script uses controllable data as the filename parameter to a file handling API. |
| Uri.LocalPath Property (System) | Microsoft Learn | public: property System::String ^ LocalPath { System::String ^ get(); }; public string LocalPath { get; } member this.LocalPath : string Public ReadOnly Property ... |