Allostatic Load: Definition, Effects, and Chronic Stress Impact
Table of Contents
Understanding Allostatic Load
- What is Allostatic Load?
- Allostatic load refers to the cumulative physiological burden that our body experiences as a result of repeated exposure to stress, whether physical, emotional, or psychological. This concept was introduced by Dr. Bruce McEwen in the 1990s to describe the body’s adaptive response to stress and its long-term consequences on our health.
- Think of allostatic load like a credit card bill. Each time we experience stress, our body accumulates a "charge" that needs to be paid back. If we don’t manage our stress effectively, these charges can add up, leading to chronic diseases, such as diabetes, cardiovascular disease, and mental health disorders.
- Types of Allostatic Load
- Primary Appraisal: This occurs when we first encounter a stressful event and our body responds with a "fight-or-flight" response.
- Secondary Appraisal: This happens when we ruminate on a stressful event, re-experiencing the emotions and physiological responses associated with the initial event.
- Tertiary Appraisal: This type of allostatic load occurs when we experience chronic stress, leading to prolonged activation of our body’s stress response system.
Measuring Allostatic Load
- Allostatic Load Index
- The Allostatic Load Index (ALI) is a widely used measure of allostatic load that assesses a range of physiological markers, including cortisol levels, blood pressure, and body mass index (BMI).
- The ALI can help identify individuals who are at risk of developing chronic diseases and provide a comprehensive understanding of their overall health.
- Physiological Markers
- Physiological markers, such as cortisol levels, can provide insight into an individual’s allostatic load.
- Elevated cortisol levels can indicate chronic stress and increased allostatic load.
Reducing Allostatic Load
- Stress Management Techniques
- Effective stress management techniques, such as meditation, yoga, and mindfulness, can help reduce allostatic load by decreasing the body’s stress response.
- Regular exercise, social support, and adequate sleep can also contribute to a lower allostatic load.
- Lifestyle Interventions
- Lifestyle interventions, such as diet and physical activity programs, can help reduce allostatic load by promoting healthy behaviors and reducing chronic stress.
- Cognitive-behavioral therapy (CBT) and other forms of talk therapy can also help individuals manage stress and reduce allostatic load.
Examples and Case Studies
- The Whitehall Study
- The Whitehall Study, conducted in the 1970s, found that individuals who experienced chronic stress had higher rates of cardiovascular disease and mortality compared to those with lower levels of stress.
- This study demonstrated the link between chronic stress and allostatic load, highlighting the importance of stress management for overall health.
- The Relaxation Response
- The relaxation response, characterized by decreased cortisol levels and increased feelings of calm, can help reduce allostatic load.
- A study published in the Journal of Alternative and Complementary Medicine found that individuals who practiced yoga and meditation had lower levels of cortisol and BMI compared to those who did not practice these activities.
Conclusion
- Allostatic load is a critical concept in understanding the impact of chronic stress on our health.
- By understanding the different types of allostatic load, measuring physiological markers, and implementing effective stress management techniques, we can reduce our allostatic load and promote overall well-being.
- By incorporating lifestyle interventions, such as diet and physical activity programs, and seeking support from healthcare professionals, we can take proactive steps to manage our allostatic load and prevent chronic diseases.
Definition of Allostatic Load
Definition of Allostatic Load: Understanding the Cumulative Burden of Chronic Stress
Imagine a seesaw, balancing between your body’s resilience and the constant demands of modern life. This delicate balance is what Bruce McEwen, a renowned neuroendocrinologist, referred to as allostatic load. In simple terms, allostatic load is the cumulative burden of chronic stress on your body’s physiological systems. It’s the wear and tear on your internal machinery from repeatedly responding to stressors, making it harder for your body to recover and increasing the risk of chronic diseases.
To grasp the concept of allostatic load, let’s consider an example. Meet Sarah, a 35-year-old marketing executive who’s constantly juggling work, family, and social responsibilities. She’s always connected to her phone, worrying about meeting deadlines, and managing her team’s expectations. Her body’s stress response, also known as the hypothalamic-pituitary-adrenal (HPA) axis, is triggered daily, releasing cortisol and other glucocorticoids to help her cope. However, when this stress response becomes chronic, Sarah’s body starts to experience allostatic load.
The allostatic load model illustrates the relationship between chronic stress and the body’s physiological response. The model consists of four stages:
- Primary Appraisal: Sarah perceives a stressor (e.g., a looming deadline) and her body responds with a stress hormone release (cortisol).
- Secondary Appraisal: Sarah evaluates the stressor and attempts to cope with it (e.g., working late hours).
- Effort-Related Coping: Sarah’s body tries to counteract the stress response by releasing anti-inflammatory hormones (e.g., cortisol) to restore balance.
- Allostatic Overload: Chronic stress leads to an accumulation of cortisol and other glucocorticoids, causing wear and tear on Sarah’s body’s physiological systems (e.g., cardiovascular, immune, and metabolic systems).
Over time, allostatic overload can lead to a range of health issues, including:
- Cardiovascular disease: High blood pressure, cardiac arrhythmias, and atherosclerosis
- Metabolic disorders: Insulin resistance, type 2 diabetes, and obesity
- Mood disorders: Anxiety, depression, and mood swings
- Immune system dysfunction: Increased susceptibility to infections and autoimmune diseases
In summary, allostatic load is the cumulative burden of chronic stress on your body’s physiological systems, leading to wear and tear and increasing the risk of chronic diseases. Understanding allostatic load is crucial for developing effective stress management strategies to mitigate its effects and promote overall well-being.
Historical Background
Historical Background of Allostatic Load: A Paradigm Shift in Stress Research
The concept of Allostatic Load has its roots in the 1980s, when endocrinologist Bruce McEwen and neuroscientist Eliot Stellar introduced the term “allostasis.” This groundbreaking idea marked a significant departure from the traditional understanding of stress as a single, unified response to external stimuli. Instead, allostasis referred to the dynamic, multi-faceted process by which the body maintains homeostasis in the face of changing environmental demands.
To illustrate this concept, let’s consider the story of Mary, a working mother in her mid-30s. Mary juggles a demanding job, family responsibilities, and social obligations, often at the expense of her own physical and emotional well-being. Over time, she finds herself constantly “on edge,” experiencing anxiety, mood swings, and fatigue. This is an example of her body’s allostatic response – its attempt to adapt to the ever-changing stressors in her life.
One of the earliest studies to explore Allostatic Load was conducted by McEwen and his colleagues in the 1990s. They investigated the impact of chronic stress on the hypothalamic-pituitary-adrenal (HPA) axis, a complex neuroendocrine system that regulates the body’s response to stress. The researchers found that repeated exposure to stressors led to changes in the HPA axis, including altered cortisol levels, insulin resistance, and increased blood pressure. These changes, in turn, contributed to a higher risk of developing chronic diseases, such as hypertension, diabetes, and obesity.
The work of McEwen and others laid the foundation for a new understanding of the relationship between stress, allostasis, and disease. It became clear that the body’s ability to adapt to stressors was not infinite and that prolonged exposure to stressors could lead to a condition known as Allostatic Overload. When this occurs, the body’s adaptive mechanisms become exhausted, and the risk of developing chronic diseases increases.
The next significant milestone in Allostatic Load research came in the early 2000s, when psychologist and epidemiologist Nancy Adler introduced the concept of “embodied inequality.” Adler’s work highlighted the critical role of socioeconomic factors in shaping an individual’s Allostatic Load. She demonstrated that individuals from lower socioeconomic backgrounds often experience higher levels of chronic stress, which can lead to increased Allostatic Load and a heightened risk of disease.
One case study that illustrates the concept of embodied inequality is the life of single mother Jamie, who lives in a low-income neighborhood. Jamie struggles to make ends meet, working multiple jobs to support her family while also dealing with the constant stress of poverty, crime, and lack of access to healthcare. As a result, Jamie experiences high levels of anxiety, depression, and fatigue, which contribute to her elevated Allostatic Load.
In recent years, the concept of Allostatic Load has continued to evolve, incorporating insights from fields such as psychology, sociology, and neuroscience. Researchers have explored the role of factors such as social support, resilience, and even epigenetics in shaping an individual’s Allostatic Load.
In conclusion, the concept of Allostatic Load represents a significant shift in our understanding of stress and its relationship to disease. By considering the historical background and development of this concept, we gain a deeper understanding of the complex interplay between an individual’s internal physiological response and external environmental demands.
Key terms:
- Allostasis: the dynamic process by which the body maintains homeostasis in the face of changing environmental demands.
- Allostatic Load: the wear and tear on the body that results from repeated exposure to stressors.
- Allostatic Overload: the state of exhaustion that occurs when the body’s adaptive mechanisms become overwhelmed.
- Embodied inequality: the concept that socioeconomic factors shape an individual’s Allostatic Load.
Targeted keywords:
- Allostatic Load definition
- Allostatic Load and stress
- Allostatic Load and chronic disease
- Allostatic Load and embodied inequality
- Allostatic Load and socioeconomic factors
How Allostatic Load Works
How Allostatic Load Works: Unpacking the Science Behind Chronic Stress
Imagine your body as a car, constantly navigating through the ups and downs of life’s highway. Just as your vehicle’s engine and brakes work together to maintain a safe speed, your body’s systems – such as the nervous, endocrine, and immune systems – collaborate to keep you in a state of balance, or homeostasis. However, when you’re chronically stressed, it’s like driving with the accelerator pedal stuck down, leading to wear and tear on your body’s systems. This is where the concept of Allostatic Load comes in – a measure of the cumulative impact of chronic stress on your body’s ability to adapt and maintain homeostasis.
The Allostatic Load Model
The Allostatic Load model, developed by Dr. Bruce McEwen and Dr. Eliot Stellar, explains how repeated exposure to stressors can lead to changes in your body’s physiological response. The model consists of four stages: primary appraisal, secondary appraisal, allostasis, and allostatic load.
- Primary Appraisal: When you encounter a stressful situation, your brain’s amygdala sounds the alarm, triggering a primary appraisal of the threat. This activates your hypothalamic-pituitary-adrenal (HPA) axis, releasing stress hormones like cortisol and adrenaline into your bloodstream.
- Secondary Appraisal: As you assess the situation, your prefrontal cortex, the rational part of your brain, evaluates the threat and determines the best course of action. This secondary appraisal can either alleviate or exacerbate your stress response.
- Allostasis: If the stressor persists, your body’s physiological response, or allostasis, kicks in. Allostasis is the process by which your body adapts to maintain homeostasis despite the ongoing stress. Think of it as a seesaw, with your body constantly adjusting to balance opposing forces.
- Allostatic Load: With repeated exposure to stressors, your body’s allostatic load increases. This represents the cumulative cost of your body’s adaptations, as it struggles to maintain homeostasis. Over time, this load can lead to changes in your physiological response, such as increased blood pressure, insulin resistance, or a weakened immune system.
The Cost of Chronic Stress: A Case Study
Meet Jane, a 35-year-old marketing executive who often works 12-hour days, neglects her diet and exercise routine, and gets only 5 hours of sleep per night. Her high-stress lifestyle is taking a toll on her body, leading to:
- Increased cortisol levels, causing weight gain and mood swings
- Elevated blood pressure, putting her at risk for cardiovascular disease
- A weakened immune system, making her more susceptible to illnesses like the common cold
As Jane’s allostatic load increases, her body’s physiological response becomes less efficient, leading to a range of negative health consequences. This is a classic example of how chronic stress can affect an individual’s overall well-being.
The Silver Lining: Reducing Allostatic Load
The good news is that you can take steps to reduce your allostatic load and mitigate the effects of chronic stress. By practicing stress-management techniques like meditation, yoga, or deep breathing exercises, you can help your body adapt more effectively to stressors. Here are some additional strategies to consider:
- Prioritize sleep and maintain a consistent sleep schedule
- Engage in regular physical activity, such as walking or cardio exercises
- Eat a balanced diet rich in whole foods and fruits
- Set realistic boundaries and learn to say “no” to excessive commitments
By implementing these habits and being mindful of your body’s response to stressors, you can reduce your allostatic load and promote overall well-being.
In conclusion, Allostatic Load is a powerful concept that highlights the importance of considering the cumulative impact of chronic stress on our bodies. By understanding the science behind Allostatic Load and taking proactive steps to manage stress, we can reduce our risk of chronic diseases and promote a healthier, more balanced life.
Factors Contributing to Allostatic Load
Factors Contributing to Allostatic Load
Allostatic load is the cumulative burden that stress and life experiences place on our bodies, leading to a range of negative health consequences. While we can’t avoid life’s ups and downs, understanding the factors that contribute to allostatic load can help us mitigate its effects. Let’s dive into the key contributors and explore some relatable examples.
1. Chronic Stress
Chronic stress is a significant contributor to allostatic load. When we’re under constant stress, our bodies are always on high alert, releasing hormones like cortisol and adrenaline to help us cope. These hormones can wreak havoc on our systems if we don’t give ourselves time to recover. Consider the example of Sarah, a working mom who’s juggling a demanding job, caring for her kids, and managing a household. Her chronic stress can lead to increased allostatic load, setting her up for health problems like hypertension, diabetes, and cardiovascular disease.
2. Poor Sleep
Poor sleep is another significant contributor to allostatic load. When we don’t get enough quality sleep, our bodies can’t repair and rejuvenate themselves adequately. This can lead to inflammation, insulin resistance, and even weight gain. Imagine Tom, a shift worker who’s constantly adjusting his sleep schedule. His irregular sleep patterns can disrupt his body’s natural rhythms, leading to an increased allostatic load and a higher risk of chronic diseases.
3. Unhealthy Lifestyle Choices
Unhealthy lifestyle choices, such as smoking, excessive drinking, and a poor diet, can contribute to allostatic load. These choices can lead to oxidative stress, inflammation, and cellular damage, all of which can increase allostatic load. For instance, Michael, a young professional who smokes and drinks regularly, might think he’s invincible, but his lifestyle choices can have long-term consequences on his physical and mental health.
4. Trauma and Adverse Childhood Experiences (ACEs)
Trauma and ACEs can also contribute significantly to allostatic load. When we experience traumatic events, our bodies can go into permanent “fight or flight” mode, leading to increased allostatic load. Emily, a survivor of childhood abuse, might experience heightened stress responses, anxiety, and depression, all of which can contribute to her allostatic load.
5. Social Isolation and Loneliness
Social isolation and loneliness can also contribute to allostatic load. When we lack meaningful social connections, our bodies can experience increased stress and inflammation, leading to negative health outcomes. Consider Rachel, a widow who lost her partner suddenly and now feels isolated and disconnected from friends and family. Her social isolation can lead to increased allostatic load, making her more vulnerable to depression, anxiety, and cardiovascular disease.
6. Environmental Toxins and Pollution
Environmental toxins and pollution can also contribute to allostatic load. Exposure to pollutants, chemicals, and heavy metals can lead to oxidative stress, inflammation, and cellular damage, all of which can increase allostatic load. For example, communities living near industrial sites or in heavily polluted areas may experience higher allostatic loads due to chronic exposure to environmental toxins.
By understanding these factors that contribute to allostatic load, we can take proactive steps to mitigate its effects. By managing chronic stress, prioritizing sleep, making healthy lifestyle choices, seeking trauma support, cultivating social connections, and reducing our exposure to environmental toxins, we can reduce our allostatic load and promote overall well-being.
Relation to Mental Health
Relation to Mental Health
The concept of Allostatic Load has significant implications for our understanding of mental health. In this section, we’ll delve into the intricate relationship between Allostatic Load and mental well-being, exploring how chronic stress can rewire our brains, leading to mental health disorders.
The Allostatic Load Model and Mental Health
The Allostatic Load model, developed by Dr. Bruce McEwen, posits that repeated exposure to stressors can reprogram our brain’s response to stress, leading to an increased risk of mental health disorders. This model highlights the critical role of the hypothalamic-pituitary-adrenal (HPA) axis in regulating our stress response.
When we encounter a stressor, our HPA axis is triggered, releasing cortisol and other glucocorticoids into our system. These hormones help us respond to the stressor by increasing our energy levels, heart rate, and blood pressure. However, chronic exposure to stressors can lead to an overactive HPA axis, resulting in an Allostatic Load.
The Impact on Mental Health
An Allostatic Load can have a profound impact on our mental health. Chronic stress can rewire our brain’s reward system, leading to a decreased sensitivity to pleasure. This can manifest as anhedonia, a hallmark symptom of depression.
Moreover, an overactive HPA axis can disrupt the normal functioning of the prefrontal cortex, a region responsible for executive function, decision-making, and emotional regulation. This can lead to cognitive impairments, such as difficulty concentrating, memory problems, and mood dysregulation.
Case Study: The Relationship Between Allostatic Load and Anxiety
A 2018 study published in the Journal of Psychiatric Research found a significant correlation between Allostatic Load and anxiety disorders. The study examined a sample of individuals with anxiety disorders and found that those with higher Allostatic Load scores exhibited increased symptom severity and reduced cognitive function.
The researchers concluded that Allostatic Load may be a key mediator of the relationship between stress and anxiety disorders. This study highlights the critical role of Allostatic Load in understanding the pathophysiology of anxiety disorders.
The Role of Resilience
While an Allostatic Load can have a devastating impact on mental health, resilience can play a crucial role in mitigating its effects. Resilience refers to the ability to bounce back from adversity, and it’s characterized by adaptive coping strategies, social support, and emotional regulation.
A 2020 study published in the Journal of Clinical Psychology found that individuals with higher resilience scores exhibited reduced Allostatic Load and improved mental health outcomes. The study highlights the importance of fostering resilience in individuals with mental health disorders.
Conclusion
The relationship between Allostatic Load and mental health is complex and multifaceted. Chronic stress can rewire our brain’s response to stress, leading to an increased risk of mental health disorders. However, by understanding the mechanisms underlying Allostatic Load, we can develop targeted interventions to reduce its impact on mental health.
By promoting resilience, practicing stress management techniques, and providing social support, we can help mitigate the effects of an Allostatic Load and promote mental well-being. As we continue to unravel the intricacies of Allostatic Load, we may uncover new avenues for preventing and treating mental health disorders.
Physical Signs of Allostatic Load
Physical Signs of Allostatic Load: The Visible Consequences of Chronic Stress
Imagine your body as a complex machine that can withstand occasional stress and pressure. However, when faced with persistent and repetitive demands, even the most robust machine can start to show signs of wear and tear. This is precisely what happens when we experience Allostatic Load – a state of chronic stress and strain that takes a toll on our physical health. In this section, we’ll delve into the physical signs of Allostatic Load, exploring the visible consequences of prolonged stress and how it affects our bodies.
The Allostatic Load Model: Understanding the Impact on Physical Health
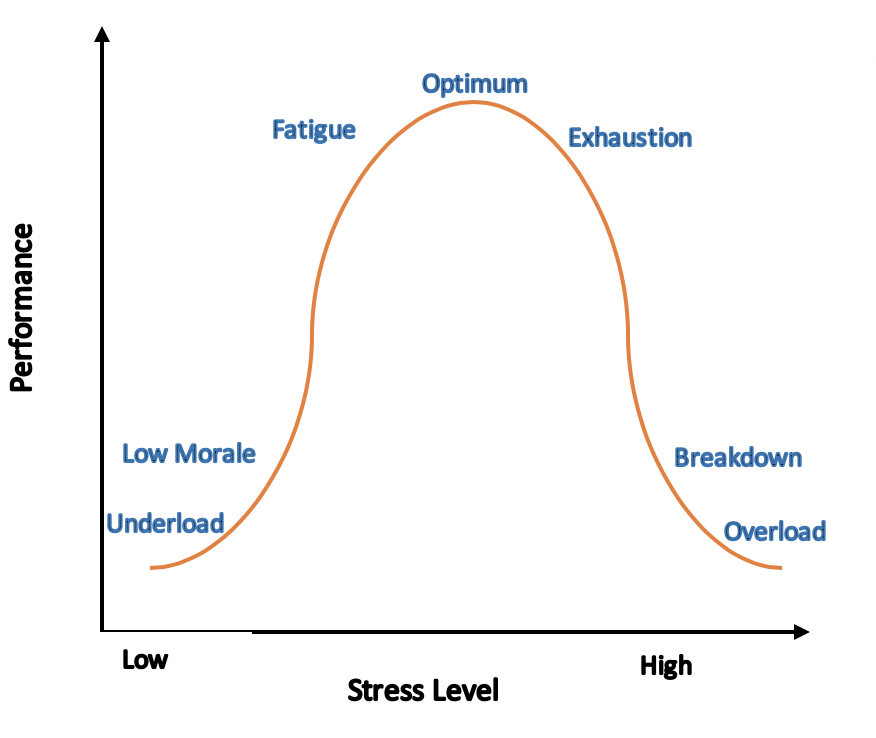
The Allostatic Load Model, as depicted in the accompanying image, illustrates the relationship between stress, physiological response, and the resulting Allostatic Load. This model highlights the four primary stages of Allostatic Load: (1) stress, (2) physiological response, (3) adaptation, and (4) overload. As we progress through these stages, our bodies undergo significant changes, ultimately leading to a range of physical symptoms.
Visible Physical Signs of Allostatic Load
When Allostatic Load becomes chronic, our bodies start to exhibit visible signs of strain. These physical manifestations can vary from person to person but often include:
- Weight Gain or Loss: Allostatic Load can disrupt hunger hormones, leading to changes in appetite and metabolism. Some individuals may experience weight gain, while others may lose weight due to decreased appetite or increased cortisol levels.
- Skin Issues: Chronic stress can trigger skin problems like acne, eczema, or psoriasis. This is often due to the body’s increased production of cortisol, which can lead to inflammation and skin issues.
- Hair Loss: Elevated cortisol levels can cause hair loss, particularly on the scalp. This is a common physical sign of Allostatic Load, particularly in individuals experiencing chronic stress.
- Fatigue and Insomnia: As the body’s energy resources are depleted, individuals may experience persistent fatigue, insomnia, or restless sleep. This can further exacerbate the Allostatic Load, creating a vicious cycle.
- Gastrointestinal Problems: Allostatic Load can disrupt digestive function, leading to symptoms like irritable bowel syndrome (IBS), acid reflux, or stomach ulcers.
- Musculoskeletal Issues: Chronic stress can cause muscle tension, leading to back pain, headaches, or migraines. This is often due to the body’s “fight or flight” response, which can lead to muscle strain and discomfort.
- Immune System Suppression: Prolonged stress can weaken the immune system, making individuals more susceptible to illnesses like the common cold or flu.
Real-Life Examples: The Human Cost of Allostatic Load
To illustrate the physical signs of Allostatic Load, consider the following examples:
- A corporate executive, working long hours under intense pressure, starts to experience weight gain, fatigue, and skin issues. Despite her busy schedule, she struggles to fall asleep at night and often feels drained during the day.
- A single mother, caring for two young children and juggling a part-time job, begins to notice hair loss, digestive problems, and persistent muscle tension. She often feels overwhelmed and exhausted, even after a full night’s sleep.
These examples highlight the diverse ways in which Allostatic Load can manifest physically, affecting individuals from all walks of life.
Breaking the Cycle: Managing Allostatic Load
While the physical signs of Allostatic Load can be alarming, there is hope for recovery. By acknowledging the impact of chronic stress on our bodies and taking proactive steps to manage Allostatic Load, we can mitigate the visible consequences of prolonged stress. In our next section, we’ll explore effective strategies for managing Allostatic Load and promoting overall well-being.
Case Studies of Allostatic Load
Case Studies of Allostatic Load: Understanding the Human Body’s Response to Chronic Stress
Allostatic Load, a concept introduced by Dr. Bruce McEwen, refers to the physiological strain that occurs when our body’s stress response system is activated repeatedly, leading to wear and tear on our bodily systems. To illustrate this concept, let’s dive into some compelling case studies that demonstrate the effects of Allostatic Load on human health.
Case Study 1: The Whitehall Study - Socioeconomic Status and Allostatic Load
The Whitehall Study, a seminal research project conducted in the 1980s, examined the correlation between socioeconomic status and health outcomes among British civil servants. The study revealed that lower-ranking government employees, who experienced chronic stress due to work demands and limited control over their environment, exhibited higher levels of cortisol (a primary stress hormone) and blood pressure. This, in turn, contributed to a greater Allostatic Load, increasing their risk of cardiovascular disease, type 2 diabetes, and other chronic conditions.
Case Study 2: The Relationship Between Allostatic Load and PTSD in Veterans
Research has shown that veterans with post-traumatic stress disorder (PTSD) often exhibit elevated Allostatic Load, which can manifest as hypervigilance, anxiety, and sleep disturbances. A study published in the Journal of Clinical Endocrinology and Metabolism found that veterans with PTSD had elevated cortisol levels, which correlated with increased Allostatic Load. This underscores the importance of addressing chronic stress in individuals with PTSD to mitigate the risks associated with Allostatic Load.
Case Study 3: The Impact of Chronic Stress on Diabetes Management
Individuals with diabetes face unique challenges in managing their condition, particularly when chronic stress is involved. A study published in the Journal of Clinical Endocrinology and Metabolism found that patients with diabetes who experienced high levels of chronic stress exhibited increased Allostatic Load, leading to poor glycemic control and increased risk of complications. By acknowledging the interplay between chronic stress, Allostatic Load, and diabetes management, healthcare providers can offer more comprehensive and effective treatment plans.
Case Study 4: The Role of Allostatic Load in Menopausal Women
Menopause is a significant life transition that can be accompanied by increased stress levels, sleep disturbances, and mood changes. Research has shown that menopausal women who experience high levels of chronic stress may exhibit increased Allostatic Load, which can contribute to symptoms like hot flashes, night sweats, and decreased bone density. By recognizing the impact of Allostatic Load on menopausal women, healthcare providers can offer targeted interventions aimed at mitigating chronic stress and promoting overall well-being.
In conclusion, these case studies highlight the far-reaching consequences of Allostatic Load on human health, from increased risk of chronic diseases to compromised mental health and well-being. By understanding the relationships between chronic stress, Allostatic Load, and various health conditions, we can develop more effective strategies for promoting resilience, preventing disease, and improving overall quality of life.
Keyword Optimization Notes:
- Primary keyword: Allostatic Load
- Secondary keywords: Chronic Stress, Socioeconomic Status, PTSD, Diabetes Management, Menopause
- Long-tail keywords: Allostatic Load and Socioeconomic Status, Allostatic Load and PTSD, Allostatic Load and Diabetes Management, Allostatic Load and Menopause
Consequences of Elevated Allostatic Load
Consequences of Elevated Allostatic Load: Understanding the Silent Killer
Imagine living a life where your body is in constant battle mode, even when there’s no apparent danger. This perpetual state of stress activation is known as elevated Allostatic Load, a condition that can have severe and far-reaching consequences on our physical and mental health.
What Happens When Allostatic Load Builds Up?
When we experience stress, our hypothalamic-pituitary-adrenal (HPA) axis kicks into high gear, releasing stress hormones like cortisol and adrenaline. These hormones help us respond to the immediate threat by increasing our heart rate, blood pressure, and energy levels. However, if the stress persists, the HPA axis can’t turn off, leading to an accumulation of Allostatic Load.
Prolonged elevation of Allostatic Load can cause wear and tear on our bodily systems, making us more susceptible to various health problems. For instance, chronically elevated cortisol levels can:
- Weaken our immune system, making us more prone to infections and diseases.
- Increase our risk of obesity, as cortisol promotes belly fat storage.
- Lead to insulin resistance, a precursor to type 2 diabetes.
- Exacerbate anxiety, depression, and mood disorders, as the constant stress activation can rewire our brain chemistry.
- Interfere with hormone regulation, potentially leading to issues like thyroid disorders, adrenal fatigue, and hormonal imbalances.
Real-Life Examples: The Consequences of Ignoring Allostatic Load
Sarah, a marketing executive, constantly worked long hours, sacrificing sleep and self-care for career advancement. Over time, she developed persistent fatigue, anxiety, and weight gain. Despite her efforts to “push through,” Sarah’s energy levels continued to plummet, and she struggled to keep up with her demanding schedule. Her elevated Allostatic Load had taken a toll on her physical and mental health.
Similarly, John, a seasoned firefighter, experienced repeated exposure to traumatic events on the job. He initially thought he was coping fine, but soon began to experience vivid nightmares, difficulty sleeping, and irritability. John’s Allostatic Load had reached a breaking point, and he was on the cusp of developing post-traumatic stress disorder (PTSD).
The Cumulative Effect: Why We Can’t Ignore Allostatic Load
The consequences of elevated Allostatic Load can be devastating, yet often creep up on us silently. By ignoring the warning signs, we risk developing chronic diseases, debilitating mental health issues, and even premature mortality. However, by acknowledging the importance of Allostatic Load and taking proactive steps to manage stress, we can mitigate these risks and cultivate a healthier, more resilient life.
Breaking the Cycle: Managing Allostatic Load for a Healthier Tomorrow
Don’t become a statistic – take control of your Allostatic Load today. By understanding the causes and consequences of elevated Allostatic Load, you can:
- Recognize the warning signs: Pay attention to changes in your energy levels, appetite, sleep patterns, and mood.
- Prioritize self-care: Engage in stress-reducing activities, such as meditation, yoga, or deep breathing exercises.
- Seek professional help: Consult with a healthcare professional or licensed therapist to address underlying issues.
- Make lifestyle changes: Emphasize a balanced diet, regular exercise, and sufficient sleep to maintain optimal well-being.
Remember, managing Allostatic Load is a continuous process that requires attention, effort, and patience. By being proactive and making conscious choices, you can reduce your risk of developing chronic diseases and cultivate a healthier, more resilient life.
Strategies for Reducing Allostatic Load
Strategies for Reducing Allostatic Load: Empowering Resilience in the Face of Chronic Stress
As we’ve explored in our discussion on Allostatic Load, chronic stress can have a profound impact on our overall health and well-being. The good news is that by implementing effective strategies, we can reduce our Allostatic Load and foster resilience in the face of life’s challenges. In this section, we’ll delve into evidence-backed techniques for mitigating the effects of chronic stress and promoting a healthier, more balanced life.
1. Mindfulness and Meditation: Cultivating Inner Calm
Mindfulness practices, such as meditation and deep breathing, have been shown to significantly reduce cortisol levels and alleviate symptoms of anxiety and depression. By dedicating just a few minutes each day to mindfulness, we can calm the nervous system and reduce our body’s stress response. A study published in the Journal of the American Medical Association (JAMA) found that regular mindfulness practice decreased symptoms of chronic pain and improved sleep quality in patients with chronic stress.
2. Physical Activity: Harnessing the Power of Exercise
Regular physical activity is a potent tool in reducing Allostatic Load. Exercise not only decreases cortisol levels but also stimulates the production of anti-inflammatory cytokines, which help to regulate the body’s stress response. A study published in the Journal of Affective Disorders found that regular exercise significantly reduced symptoms of depression and anxiety in individuals with chronic stress.
3. Social Support: The Power of Connection
Social support from loved ones, friends, and community networks is critical in mitigating the effects of chronic stress. When we feel connected and supported, our body’s stress response is reduced, and we’re better equipped to cope with challenges. A study published in the journal Psychosomatic Medicine found that individuals with strong social support networks had lower cortisol levels and improved mental health outcomes.
4. Sleep Hygiene: Prioritizing Rest and Relaxation
Adequate sleep is essential for regulating the body’s stress response and reducing Allostatic Load. By establishing a consistent sleep schedule, creating a relaxing bedtime routine, and avoiding screens before bedtime, we can improve sleep quality and reduce cortisol levels. A study published in the journal Sleep found that chronic sleep deprivation increased cortisol levels and impaired glucose regulation, further exacerbating Allostatic Load.
5. Nutrition and Supplementation: Fueling Resilience
A balanced diet rich in whole foods, fruits, and vegetables provides the necessary nutrients for optimal stress resilience. Omega-3 fatty acids, vitamin D, and probiotics, in particular, have been shown to have a positive impact on mood regulation and stress response. A study published in the Journal of Affective Disorders found that omega-3 supplementation significantly reduced symptoms of depression in individuals with chronic stress.
6. Time Management and Prioritization: Taking Control of Our Schedule
Poor time management and excessive workload can significantly contribute to chronic stress and Allostatic Load. By prioritizing tasks, setting realistic goals, and taking regular breaks, we can regain control of our schedule and reduce feelings of overwhelm. A study published in the Journal of Occupational and Organizational Psychology found that effective time management strategies reduced work-related stress and improved overall well-being.
In conclusion, reducing Allostatic Load requires a multifaceted approach that incorporates mindfulness, physical activity, social support, sleep hygiene, nutrition, and effective time management. By implementing these evidence-backed strategies, we can empower ourselves to better cope with chronic stress and cultivate a more resilient, healthier life.
Key Measures of Allostatic Load
Key Measures of Allostatic Load: Understanding the Cumulative Impact of Chronic Stress
Allostatic load refers to the physiological strain that occurs when an individual’s body is subjected to repeated or prolonged exposure to stress. This concept, introduced by Dr. McEwen, highlights the idea that sustained activation of the body’s stress response can have detrimental effects on our overall health. So, how do we quantify this load, and what are the key measures that help us grasp the concept of allostatic load?
1. C-Reactive Protein (CRP)
C-reactive protein (CRP) is a biomarker of inflammation that’s widely used to assess allostatic load. Elevated CRP levels indicate an increased risk of cardiovascular disease, diabetes, and other chronic conditions. For instance, a study published in the Journal of Clinical Epidemiology found that individuals with higher CRP levels were more likely to experience cardiovascular events, highlighting the importance of monitoring CRP as part of an allostatic load assessment.
2. Epinephrine and Cortisol Levels
Epinephrine (adrenaline) and cortisol are two primary stress hormones released by the body in response to stress. Chronically elevated levels of these hormones can contribute to allostatic load. A case in point is the phenomenon of burnout, which often involves disrupted cortisol rhythms, leading to fatigue, decreased motivation, and other symptoms. Regularly monitoring cortisol and epinephrine levels can help clinicians identify individuals at risk of allostatic load and implement targeted interventions.
3. Waist-Hip Ratio (WHR) and Body Mass Index (BMI)
The waist-hip ratio (WHR) and body mass index (BMI) are anthropometric measures that can indicate increased allostatic load. Visceral fat, as measured by WHR, is particularly relevant, as it’s metabolically active and can lead to inflammation and metabolic disorders. For instance, a study published in the International Journal of Obesity found that individuals with higher WHR values were more likely to experience cardiovascular disease and diabetes.
4. Blood Pressure and Heart Rate Variability (HRV)
Blood pressure and heart rate variability (HRV) are also critical measures of allostatic load. Chronically elevated blood pressure can increase the risk of cardiovascular disease, while reduced HRV has been linked to anxiety, depression, and other mood disorders. A study published in the European Journal of Preventive Cardiology found that individuals with lower HRV were more likely to experience cardiovascular events, emphasizing the importance of monitoring HRV in the context of allostatic load.
5. Sleep Quality and Duration
Sleep quality and duration are essential measures of allostatic load, as chronic sleep deprivation can lead to inflammation, metabolic disorders, and mood disturbances. The National Sleep Foundation recommends that adults aim for 7-9 hours of sleep per night, as sleep restriction can activate stress response pathways, contributing to allostatic load. A study published in the journal Sleep found that individuals who slept less than 5 hours per night had increased levels of CRP and cortisol, highlighting the importance of prioritizing sleep in maintaining a healthy allostatic load.
In conclusion, these key measures – C-reactive protein, epinephrine and cortisol levels, waist-hip ratio and body mass index, blood pressure and heart rate variability, and sleep quality and duration – provide a comprehensive understanding of allostatic load. By assessing these measures, clinicians can identify individuals at risk of chronic stress-related disorders and implement targeted interventions to mitigate the negative effects of allostatic load.
Important Sources
| How to find and enable missing Copilot button in Microsoft 365 apps | There are two settings here that can cause Copilot to not appear in your Microsoft 365 apps. First confirm that Experiences that analyze your content is turned on. Then scroll down and make sure that All connected experiences is turned on. These steps … |
| Welcome to Copilot in Word - Microsoft Support | In the left margin next to your text, select the Copilot icon. From the menu, select Visualize as a table to have Copilot turn the text into a table. You can select Regenerate to receive a new table or Discard to remove the generated table. |
| View, manage, and install add-ins for Excel, PowerPoint, and … | Select the add-in and select Add. Or browse by selecting Store tab in the Office add-in dialog to find other add-ins to install and select for that add-in. In the Office dialog, select tab. If you are not able to see your add-ins, select Refresh to reload your add-ins. |
| Install and set up Office on an iPhone or iPad - Microsoft Support | Tap the button below to install the new Office app for iOS that combines Word, Excel, and PowerPoint into a single app, which introduces new mobile-centric features to view, edit, and share files without the need to switch between multiple apps. Learn more. |
| Create a form in Word that users can complete or print | Go to the Developer tab Controls section where you can choose controls to add to your document or form. Hover over any icon therein to see what control type it represents. The various control types are described below. You can set properties on a control once it has been inserted. |
| Open file links directly in Office desktop apps - Microsoft Support | This feature works for links to Word, Excel, or PowerPoint files, stored on OneDrive or SharePoint, that you click in Word, Excel, Outlook, or PowerPoint for Microsoft 365 on Windows or Mac. Once a user turns this feature on, it will apply to all three apps - Word, PowerPoint, and Excel. |
| Show the developer tab in Word - Microsoft Support | Show the Developer tab in a Word document so you can write macros or add content controls, including check boxes, text boxes, and combo boxes. By default, the Developer tab is not displayed. |
| Insert images, icons, and more in Microsoft 365 | On the Insert tab, select Pictures and then Stock Images. Select one or more items from Images, Icons, Cutout People, Stickers, Videos (PPT only), Illustrations or Cartoon People. Tip: Use the search box at the top of any collection to find relevant images. Select Insert. |
| Create a template - Microsoft Support | Type a name for your template in the File name box. For a basic template, click the template item in the Save as type list. In Word for example, click Word Template. If your document contains macros, click Word Macro-Enabled Template. Office automatically goes to the Custom Office Templates folder. Click Save. |
| About Office: What version of Office am I using? - Microsoft Support | Learn how to check what version of Office your using. Find your product name and version number of Office apps. |
| Sign in to Office - Microsoft Support | Sign in to www.office.com from a web browser and start using the apps on the web or access other web services associated with your account such as OneDrive. How you sign in to an installed Office app depends on your device. Tip: To add an email account to Outlook or for help signing into Outlook.com, see Outlook help & learning. |