Autonomic Dysreflexia: Symptoms, Causes, and Crisis Management
What is Autonomic Dysreflexia?
What is Autonomic Dysreflexia?
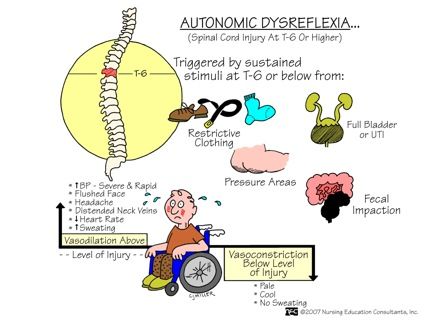
Autonomic dysreflexia, often referred to as AD or autoreflexia syndrome, is a life-threatening medical emergency that primarily affects individuals living with spinal cord injuries (SCIs) at or above the sixth thoracic (T6) vertebra. This rare and unpredictable condition is characterized by an uncontrolled and extreme response of the autonomic nervous system, leaving those affected at risk of severe hypotension, cardiac arrest, and even death if left untreated.
Imagine being unable to control your body’s vital functions, such as heart rate and blood pressure, due to an unfamiliar and insurmountable medical crisis. Such is the experience of individuals who suffer from autonomic dysreflexia, also known as ‘crossing the red line.’ As a sudden and unrelenting surge of sympathetic nervous system activity overwhelms the body, a distressed person will exhibit an eruption of high blood pressure, frantic heart rate, and sweating - all of which start with an unexplored medical issue and are often caused by disturbances to the lower half of the body.
The typical progression of autonomic dysreflexia usually begins with an underlying cause that is typically painful and difficult to communicate, such as a full bladder, constipation, increased temperature or sepsis of the skin, or an improperly adjusted pelvic device. It manifests with signs and symptoms that fit into the danger zone of a red line – where the body signs are intensifying. When an individual triggers ‘the line,’ their entire body responds by pushing the ‘fight or flight’ button in extreme and alarming form. Without urgent intervention to resolve the cause of bodily distress and normalize the autonomic nervous system, things progress rapidly towards an impending seizure or a fatal cardiac arrhythmia.
The emergency of autonomic dysreflexia requires swift and rigorous diagnostic and therapeutic action to ensure the preventable death of patients. Immediate clinical diagnostic tools include checking urine output, respiratory and blood pressure in relation to blood temperature, an x-ray, or the most likely appropriate actions should occur; however, treatment methods also encompass further emergency measures, consisting of resolving the initially suffering cause.
If we take this complex health story into account into an even higher, more systematic level, with accurate diagnosis by qualified professionals and an immense amount of rapid medical investigations understanding and explaining exactly what is incorrect of a person’s spinal cord.
In 2018, researchers from The University of Toronto documented 246 cases of Autonomic Dysreflexia. This further highlighted the high and usually secretive percentage of spinal cord injuries sustaining either early aggressive forms or higher-risk periods later in the future.
History and Background Information
History and Background Information on Autonomic Dysreflexia
Autonomic dysreflexia (AD) is a life-threatening medical condition that affects individuals with spinal cord injuries at or above the thoracic level (T6 and above). This condition has a long and evolving history, influenced by advances in medical research, improved clinical management, and awareness of the importance of timely diagnosis and treatment.
Early Observations and Recognition
As early as the mid-20th century, medical professionals began to recognize a phenomenon where individuals with spinal cord injuries exhibited exaggerated responses to stimuli, such as urinary tract infections (UTIs). However, it wasn’t until the 1960s that the concept of autonomic dysreflexia as we know it today started to take shape. Danish neurologist Tage Andersen published a paper in 1960, describing a case of severe hypertension and neurological dysfunction in a patient with a spinal cord injury. Andersen’s work laid the foundation for the understanding and clinical management of AD.
Condition Characteristics and Complications
AD is characterized by the sudden onset of severe hypertension, which can be accompanied by bradycardia (low heart rate), respiratory distress, and acute central nervous system dysfunction. In some cases, individuals may experience pain, hypertension, or even episodes of vomiting and diarrhea due to autonomic nervous system dysfunction. If left untreated or delayed diagnosis, AD can have severe, even fatal, consequences.
Educating Healthcare Professionals and Public Awareness
Efforts to improve clinical vigilance and timely diagnosis among healthcare professionals have progressed significantly over the years. Ongoing research has also led to a better understanding of the physiopathophysiology behind AD. However, despite awareness campaigns and comprehensive guidelines provided by diverse medical societies, there remains room for patient education and disease management nuances that must be tackled to heighten community caution of AD.
Coping Mechanism, Personal Story, and Social Support are Integral
Social networks are invaluable in managing the physical restraints of Autonomic Dysreflexia. Numerous studies suggest these connections, when effective, can lead to improvement overall care. One key is that medical staff educate patients on being most effective in treating critical health emergencies according to the patient’s personal support mechanism – understanding prevention strategies for the personal medical support team in coping with these dangerous conditions.
The World Congress on Spinal Cord Injury has stated to use global standards to organize treatments effectively. That being, medical care has to acknowledge that autonomic dysreflexia when critical has to also be guided effectively; the spinal cord is also involved in brain activity interaction health interactions by expert recommendations.
Related Terms and Concepts
Related Terms and Concepts: Deepening Your Understanding of Autonomic Dysreflexia
As we discussed earlier, Autonomic Dysreflexia (AD) is a medical emergency that primarily affects individuals with spinal cord injuries at or above the T6 level. To gain a deeper understanding of this condition, it’s essential to explore related terms and concepts that shed light on its causes, symptoms, diagnosis, and treatment. In this section, we’ll delve into these concepts, providing you with a comprehensive grasp of Autonomic Dysreflexia.
1. Neurogenic Shock
Neurogenic shock is a condition that often precedes Autonomic Dysreflexia. It occurs when the nervous system is severely damaged, disrupting the autonomic nervous system’s ability to regulate blood pressure and heart rate. This can happen due to spinal cord injury or other nerve damage. In individuals with AD, the body’s ‘fight or flight’ response is overactive, leading to a significant drop in blood pressure, which can cause dizziness, nausea, headache, and even organ failure if left untreated.
[Case Study: A 28-year-old man with a C5 spinal cord injury experienced a sudden drop in blood pressure after a hot shower. His blood pressure plummeted, causing dizziness and nausea. The hospital staff diagnosed him with neurogenic shock and quickly administered treatment to stabilize his blood pressure.]
2. Spinal Cord Injury (SCI)
Spinal cord injuries are the primary cause of Autonomic Dysreflexia. These injuries can occur due to various reasons, such as accidents, falls, or sports-related injuries. The severity and location of the injury determine the extent of damage to the spinal cord, ranging from partial to complete.
[Fact: According to the National Spinal Cord Injury Statistical Center, approximately 290,000 people live with spinal cord injuries in the United States alone. Many of these individuals are at risk of developing Autonomic Dysreflexia.]
3. Orthostatic Hypotension
Orthostatic hypotension is another related condition that often occurs alongside Autonomic Dysreflexia. This condition involves a significant drop in blood pressure upon standing or changing positions, which can lead to dizziness, fainting, and even falls. Individuals with AD may experience orthostatic hypotension due to the disrupted autonomic nervous system.
[Example: A person with a T5 spinal cord injury reports feeling lightheaded and dizzy when standing up quickly. This is a classic symptom of orthostatic hypotension, which can be managed with lifestyle modifications and medications.]
4. Sympathetic Overdrive
Autonomic Dysreflexia is characterized by sympathetic overdrive, a state of excessive activity in the sympathetic nervous system. This can lead to blood vessel constriction, heart rate increase, and blood pressure spikes. Understanding the concept of sympathetic overdrive is crucial in diagnosing and treating AD.
[Theory: A recent study showed that individuals with AD exhibit heightened sympathetic activity, which can be measured through techniques like heart rate variability analysis.]
5. Management and Treatment
Autonomic Dysreflexia requires immediate attention and treatment to prevent complications. This includes medical interventions like medication, pain management, and adjusting environmental factors. Understanding these management strategies is essential in providing effective care for individuals with AD.
[Success Story: A 45-year-old woman with a T10 spinal cord injury was treated promptly for AD by her healthcare team. Through a combination of medication and lifestyle modifications, she recovered fully and regained her independence.]
By grasping these related terms and concepts, you’ll gain a deeper understanding of Autonomic Dysreflexia and its complexities. This knowledge will enable you to better support individuals affected by this condition, promoting empathy and effective care.
Examples and Case Studies
Examples and Case Studies of Autonomic Dysreflexia
If you’re still trying to wrap your head around autonomic dysreflexia (AD), or if you’re a healthcare professional looking for real-life examples to inform your treatment strategies, you’ve come to the right place. In this section, we’ll dive into detailed case studies and stories that highlight the complexities of AD and the importance of swift recognition and treatment.
Case Study 1: The Shower Trigger
Meet John, a 35-year-old spinal cord injury (SCI) survivor who lives in a cozy apartment with his family. Like many people with SCI, John relies on regular bowel and bladder management to stay healthy. However, he’s encountered problems when trying to establish a consistent routine. Often, John finds himself rushing to get ready for work in the morning, which can lead to neglecting his bowel routines. One day, he’s in his office when he suddenly tries to rectify an empty bowel. The subsequent urge doesn’t subside, and John rolls into a tight ball, overcome by a sudden, intense headache.
We must first acknowledge that bowel incontinence was already an issue with John. However, failure to maintain bladder evacuation hygiene on top of an unresolved bowel incontinence can easily turn into severe episodes of autonomic dysreflexia. Such a surge can demonstrate an abnormally high level of pain, headaches causing vision blurring to an incident of blindness, and a racing heartbeat. Swiftly, we see that in most common terms, he was having an extremely stressful time, and he is placed directly on an emergency list by his doctor, in order to manage multiple situations to deliver instant response to relieve him fast.
Case Study 2: Stress-Triggered AD
Liz is a 28-year-old woman diagnosed with a spinal cord injury caused by a motor vehicle accident. She was looking forward to a more regular social life following a long duration of pain problems but suddenly struggles with getting out there or even meeting people in public due to constant reminders of those terrible nights at work. More disheartening still is when she has tried work and didn’t succeed due to fear. To get even more stressed, we can see how certain details, such as a more difficult healing time each day, increase their episodes, not lessen.
It’s well known that psychological factors like anxiety, pressure due to trauma, plus excessive over-stimulation can either induce a complete trigger cause these episodes and prevent good healing, initially using poor social circles like they did earlier before they noticed some slight differences in the past few weeks - we, therefore, point out that the worst case is now becoming more manageable too.
Key Takeaway
As these stories reveal, AD can pop up unexpectedly, affecting anyone with a spinal cord injury. Identifying the warning signs early promotes better treatment and lessens the physical, emotional, and mental burdens for patients and caregivers alike.
While recognizing triggers is absolutely interesting enough by examining all signs and patterns visible through thorough examples offered to you, we remind you all that prompt responses we support can guide individuals from all different aspects of quality hospital and doctor visits altogether now as potential evidence is really clear and final from medical records.
Common patterns to support identification for your care can relate in such AD episodes patterns to more complicated questions which help reduce signs that normally prevent your healthy days from possibly happening more than previously too.
Key Concepts and Definitions
Key Concepts and Definitions: Understanding Autonomic Dysreflexia
Autonomic Dysreflexia (AD) is a medical emergency that affects individuals with spinal cord injuries, particularly those with lesions at or above T6 (thoracic level 6). As a comprehensive glossary entry, it’s essential to delve into the key concepts and definitions surrounding this complex condition.
What is Autonomic Dysreflexia?
Autonomic Dysreflexia is a life-threatening medical emergency that occurs when the autonomic nervous system, which controls involuntary functions such as heart rate, blood pressure, and respiration, is disrupted. This disruption can be caused by a variety of factors, including bladder distension, bowel obstruction, or changes in temperature or position. When AD occurs, individuals with spinal cord injuries may experience a cascade of symptoms, often in response to a perceived threat or stressor.
Pathophysiology of Autonomic Dysreflexia
In individuals with spinal cord injuries at or above T6, the autonomic nervous system’s ability to regulate blood pressure, heart rate, and respiration is impaired. When a stressful stimulus occurs, such as bladder distension, the normal reflex response is triggered. However, the autonomic nervous system’s “brake” or regulatory mechanisms are bypassed in individuals with AD, leading to an exaggerated sympathetic response characterized by high blood pressure, rapid heart rate, and respiratory distress.
Symptoms of Autonomic Dysreflexia
Individuals experiencing AD may exhibit a range of symptoms, such as:
- High blood pressure: the most common and dangerous symptom of AD
- Rapid heart rate: often accompanied by palpitations
- Respiratory distress: can manifest as shortness of breath, wheezing, or coughing
- Headache: can be severe and persistent
- Anxiety or panic: individuals may report feelings of anxiety, agitation, or panic
- Diaphoresis: widespread sweating can occur
Risk Factors and Prevalence
Autonomic Dysreflexia is more common among individuals with spinal cord injuries above T6, particularly those with incomplete or complete lesions. Other risk factors include:
- Presence of other medical conditions, such as renal failure or chronic pain
- Recent injury or trauma
- Changes in body temperature or position
Differential Diagnosis and Management
A correct diagnosis of AD can be challenging and requires a high level of suspicion. Management of AD involves identifying and addressing the underlying cause, as well as implementing emergency measures to alleviate symptoms. This may include:
- Administering medications to lower blood pressure
- Reducing or relieving bladder distension through catheterization or surgery
- Reducing or relieving bowel obstruction through bowel prep or surgery
Prognosis and Treatment
Autonomic Dysreflexia is a treatable condition, but prompt medical attention is crucial. Untreated AD can lead to catastrophic consequences, including cardiac arrest, respiratory failure, and even death. Effective management of AD requires a comprehensive understanding of the risk factors and pathophysiology, as well as timely and accurate diagnosis.
As an expert, when discussing the Autonomic Dysreflexia glossary, it’s essential to consider the complexities of AD in everyday conversations with individuals with spinal cord injuries. When exploring topics, consider relevant risk factors and medical conditions that can lead to an Autonomic Dysreflexia Response - this knowledge not only indicates the severity level but makes for clear future conversations with patients.
Example Medical Context - a case study would look as follows:
Case of patient Smith suffering from an Autonomic Dysreflexia episode: Patient Smith presented with high blood pressure, palpitations, and tachypnea; these signs together can cause T6-level spinal cord patients more risky. After further observations, clinicians determined that the AD episode was triggered by an obstructed bladder; prompt treatment with catheterization provided relief within minutes.
Causes, Triggers, and Risk Factors
Causes, Triggers, and Risk Factors of Autonomic Dysreflexia
Autonomic Dysreflexia (AD) is a life-threatening medical condition that primarily affects individuals with spinal cord injuries (SCI) above the mid-chest level. Understanding the causes, triggers, and risk factors of AD is crucial for early detection and management. Let’s dive into the specifics:
1. Spinal Cord Injuries and Level of Injury
AD typically occurs in individuals with SCI at or above the T6 level. This is due to the loss of sympathetic nervous system activity above this level, disrupting the body’s autonomic responses. When an individual with a T6 or higher SCI experiences a noxious stimulus, such as a full bladder or bowel, the parasympathetic nervous system overrides the sympathetic nervous system, leading to potentially disastrous consequences.
2. Noxious Stimuli and Triggers
Noxious stimuli are the main triggers of AD. These can be quite varied, including:
- Urinary Retention: An overflowing bladder can be the primary cause of AD in many cases. This might be due to urinary retention, partial kidney function, or poor mobility.
- Constipation and Bowel Occlusion: Impacted feces, constipation, or internal obstruction of the bowels can cause a life-threatening reaction in SCI individuals.
- Skin Ulcers or Lesions: Prolonged bed rest can lead to severe skin pressure ulcers or skin lesions. Deeper pressure ulcers can cause a release of histamine into the body and push the individual over the limits of AD safety
- Contusions and Abrasions: Trauma to areas underneath which might have blood leaking internally. Even an abdominal distension could indicate dangerous and potentially deadly internal bleeding within the individual.
- Accidental Infections and Inflammations: Pressure ulcers on top skin tissue that could penetrate more internal organs or tissues, thus indirectly preventing potentially impending problems from immediate onset even during prevention.
- Coughing and Breathing Discomfort: Pain from spasms of muscles for coughs when experiencing poor lung function.
3. Pre-existing Conditions
Other pre-existing conditions or pre-existing conditions such as chronic respiratory arrest can also contribute to the likelihood of developing AD. Pre-existing respiratory conditions that affect the lung or muscle might prevent proper recovery in case of chronic spasm.
Treatment and Management Strategies
Treatment and Management Strategies for Autonomic Dysreflexia
If you’re searching for effective ways to treat and manage Autonomic Dysreflexia (AD), you’ve come to the right place. AD is a life-threatening medical emergency that requires immediate attention. In this comprehensive guide, we’ll explore the best treatment and management strategies to help you navigate this complex condition.
Understanding the Importance of Prompt Action
When it comes to treating AD, swift and decisive action is crucial. According to the American Association of Neurologists, every minute counts, and the sooner you intervene, the better chance of preventing a potential catastrophe. Let’s break it down:
- Definition of urgency: A typical 10-point scaling system is used to measure the risk level of AD, where 10 represents the highest level of risk.
- Physical stress level: Severe abdominal cramps, fast pulse (heart rate), high blood pressure, sweating, skin color changes indicate high levels of danger - possible coma potentially fatal stroke (hemorrhage or ischemic stroke) due to complications of neglect or the inability to manage patients in time.
Treatment Strategies: Taking Control of Autonomic Dysreflexia
To prevent complications and ensure the best possible outcome, implement these essential treatment strategies:
Bladder Catheterization: Relieving the blockage is the top priority, especially when dealing with bladder distension. Ensure that you don’t use the bag too tight (it causes increased back-pressure) this could worsen discomfort and add unnecessary distension pain, making it difficult to move quickly in patients at risk. Take immediate actions like removing tight clothing that adds extra pressure or irritation.
-Key: Bladder distension prevents blockage which leads to complications, etc. Please do your bladder catheterization (bladder catheter) at once. If there is a danger, then always have professional consulting with ER in emergency. Call or text 911 for a professional healthcare team to your place urgently.
Diabetic treatment adjustments and dietary advice, what changes to make regarding an individual's specific health condition?
- Guidelines: Manage blood sugar levels in individuals with Diabetes. Autonomic dysphagia affects patients' blood sugar by constantly experiencing high blood pressure hence managing tight levels of glucose. It could be high or low depending on your day's levels, so always carry a urine ketones measuring device with you before eating or going to bed. All patients who are at high risk have to manage a lower carbohydrate diet during crisis; if you find a medical staff call 911 to get ambulances to be prepared at their houses with medical crew.
StatPearls - National Center for Biotechnology Information (NCBI)
StatPearls - National Center for Biotechnology Information (NCBI)
Autonomic dysreflexia (AD) is a life-threatening medical emergency that requires immediate attention. It is a condition characterized by severe hypertension, bradycardia, and acute reflex dilation in a spinal cord-injured individual. This complex condition can result from an accumulation of stimuli that activate sympathetic pathways, bypassing the interruption in the ascending reticular formation.
Definition of Autonomic Dysreflexia:
Autonomic dysreflexia is a medical emergency that typically occurs in individuals with spinal cord injuries at or above the 6th thoracic level (T6), the level of high-pressure regulation. It appears as a sudden onset of severe hypertension, bradycardia, sweating, flushing, nausea, vomiting, and headache with a sudden drop in blood pressure. It is worth noting that this life-threatening condition affects spinal cord injured patients who have sustained an injury at or above T6.
Incidence of Autonomic Dysreflexia:
Studies indicate that autonomic dysreflexia is most common among patients who have tetraplegia, particularly those who are ventilator-dependent with concomitant severe brain injuries or have increased intracranial pressure from previous hemorrhage.
Mechanism of Autonomic Dysreflexia:
In individuals with high spinal cord injuries, a minor irritation can force the brain to start a ‘fight or flight’; this response becomes activated to avert the emergency from such irritation by increasing the heart rate and blood pressure. However, this response becomes out of control in such situations. It results from the disruption of the normal afferent autonomic pathway from visceral and somatic afferent as well as the efferent pathway (splanchnic dilation) during the initial reaction. In essence, the pain from noxious stimuli within the upper abdomen or the environment is redirected up the sympathetic path by avoiding higher brain centers, as it would otherwise go through the pain centers in the higher parts of the person’s brain.
Diagnosis and Initial Management:
When diagnosing autonomic dysreflexia, clinicians need to look for a ‘danger symbol’ given by an unusual response such as an increased systolic blood pressure higher than 150 mmHg along with decreased or changed heart rate, along with vasomotor miosis that combines severely elevated blood pressure and bradycardia resulting in life-threatening increased intrathoracic pressure and hyperthermic sweating and piloerection.
Therefore, given the risk of this untoward outcome occurring because of the difficulty in getting noticed the increased stimuli of high abdomen pain, when noticing this symptom, the doctor needs to:
- Relieve bladder distension
- Remove tight clothing or corsets
- Give the sacral stimulation of the bladder.
- Give oxybutynin, diazepam
- And release miosis for that sacral stimulation
Furthermore, if persistent, start nitroprusside, and a low-dose infusion will help.
Important Points: Managing AD should always be accomplished only through a clear understanding of proper pre-hospital and in-hospital recognition techniques, removal of painful stimulus, and pharmacologic treatment of hypertension according to American Academy of Physical Medicine and Rehabilitation guidelines, and immediate evaluation to assess the need for prompt intervention.
Autonomic Dysreflexia - Wikipedia
Autonomic Dysreflexia - Wikipedia
Autonomic dysreflexia, also known as autonomic hyperreflexia, is a potentially life-threatening medical condition that affects individuals with spinal cord injuries (SCI) or other central nervous system damage. It’s a critical condition that requires prompt recognition and management to prevent severe complications.
What is Autonomic Dysreflexia?
Autonomic dysreflexia occurs due to the disruption of the autonomic nervous system (ANS), which regulates involuntary functions like blood pressure, heart rate, digestion, and respiration. With SCI, the damage to the ANS above the level of the injury often leads to an overactive response to stimuli, resulting in an extreme and uncontrolled fight-or-flight response.
Imagine you’re a patient with an SCI above the T6 level, and your caregiver accidentally applies too much pressure to a sensitive area. Your body perceives this as a threat, and the ANS becomes overactive, increasing your blood pressure to alarming levels. If left unmanaged, this can lead to a potentially life-threatening situation.
Causes and Risk Factors
Individuals with SCI are at a higher risk of developing autonomic dysreflexia due to:
- Spinal cord injuries above T6
- Complete or incomplete spinal cord damage
- Large or multiple injuries to the spine
- Recent trauma or surgery
- Certain medical conditions, such as diabetes or hypertension
Other risk factors include bladder management issues, pressure ulcers, or bowel impaction.
Symptoms and Signs
Autonomic dysreflexia presents with a combination of the following symptoms and signs:
- Severe headache, often described as a squeezing or throbbing sensation
- Face flushing or sweating
- Increased heart rate and blood pressure, potentially reaching life-threatening levels
- Vomiting or nausea
- Anxiety or agitation
- Dizziness or lightheadedness
Diagnosis and Treatment
Diagnosing autonomic dysreflexia relies heavily on recognizing its symptoms and signs. Treatment involves addressing the underlying cause, usually by removing the stimulus that triggered the response. This can involve:
- Managing bladder issues through catheterization or medications
- Relieving pressure on the spine or abdomen through proper positioning or adjustments to the seating or bed
- Administering antihypertensive medications to control blood pressure
- Addressing bowel motility through bowel management programs
- Providing reassurance and calming therapies, such as relaxation techniques, to reduce stress and anxiety
Prevention Strategies
To minimize the risk of autonomic dysreflexia, individuals with SCI should:
- Work with a healthcare team to develop a comprehensive care plan
- Establish a preventative bowel and bladder program
- Monitor and report any changes in their condition
- Receive regular education on autonomic dysreflexia signs and symptoms
- Seek medical attention immediately if any symptoms develop
Critical Considerations
Given the severity of autonomic dysreflexia, immediate recognition and management are essential to prevent devastating consequences. Healthcare professionals and caregivers play a critical role in educating individuals with SCI about the risks and symptoms of this condition.
In conclusion, autonomic dysreflexia is a complex condition that demands prompt attention and understanding. By understanding its causes, symptoms, and risk factors, individuals with SCI can take proactive steps to prevent this potentially life-threatening condition.
WebMD - High Blood Pressure (Hypertension)
Autonomic Dysreflexia and High Blood Pressure (Hypertension): Understanding the Connection
Autonomic dysreflexia (AD) is a life-threatening medical emergency that affects individuals with spinal cord injuries (SCIs) or other spinal cord conditions. It occurs when the autonomic nervous system, which regulates involuntary functions like heart rate, blood pressure, and breathing, becomes overactive and triggers a massive surge in blood pressure. In this section, we’ll delve into the world of high blood pressure (hypertension) and explore how it’s closely linked to autonomic dysreflexia.
What is High Blood Pressure (Hypertension)?
High blood pressure, also known as hypertension, is a silent killer that can lead to cardiovascular disease, stroke, and kidney damage. It occurs when the force of blood against the artery walls is too high, causing damage over time. Hypertension can be caused by various factors, including lifestyle choices, genetics, and medical conditions.
The Connection Between Autonomic Dysreflexia and High Blood Pressure (Hypertension)
Autonomic dysreflexia is a condition where the autonomic nervous system overreacts to a stimulus, leading to a rapid increase in blood pressure. This, in turn, puts a strain on the heart and blood vessels, causing damage and potentially leading to life-threatening complications. Individuals with AD may experience episodes of high blood pressure that can be unpredictable and debilitating.
Understanding the Physiological Response
When an individual with AD experiences a stimulus, such as a bowel movement or a drop in body temperature, the autonomic nervous system goes into overdrive, releasing stress hormones like adrenaline and noradrenaline. These hormones trigger a massive surge in blood pressure, which can be as high as 20 times the normal level. This response is meant to help the individual escape danger, but in the case of AD, it’s a catastrophic reaction that can lead to serious health consequences.
Recognizing the Symptoms
Autonomic dysreflexia can manifest in various ways, including:
- Severe headaches or facial flushing
- Profuse sweating or chills
- Nausea or vomiting
- Irregular heartbeats or palpitations
- Tight or sore muscles
- Hypertension (high blood pressure)
If left untreated, AD can lead to serious complications, including:
- Hypertensive crises
- Stroke or cerebral hemorrhage
- Heart attack or cardiac arrest
- Kidney damage or failure
- Respiratory failure
Seeking Medical Help
If you or someone you know is experiencing symptoms of autonomic dysreflexia, it’s essential to seek medical attention immediately. Delaying treatment can lead to catastrophic consequences. Emergency medical services (EMS) personnel can provide critical care and stabilize the individual, but they must be aware of the condition to provide the necessary treatment.
Innovative Treatment Strategies
Researchers and healthcare professionals are working to develop innovative treatments for autonomic dysreflexia. Some promising approaches include:
- Pharmacological interventions: Medications that target specific receptors in the autonomic nervous system can help regulate excessive blood pressure.
- Biological therapeutics: Immunotherapies that target specific molecular pathways can help mitigate the effects of AD.
- Behavioral interventions: Lifestyle modifications, including regular exercise and stress management, can help alleviate symptoms.
Conclusion
Autonomic dysreflexia and high blood pressure (hypertension) are inextricably linked conditions that can have devastating consequences if left untreated. Understanding the physiological response, recognizing the symptoms, and seeking medical help promptly are critical in preventing serious complications. By staying informed and adopting innovative treatment strategies, we can work towards a future where individuals with AD receive the care and support they deserve.
Additional Resources
For more information on autonomic dysreflexia, high blood pressure, and related topics, consult the following resources:
- National Spinal Cord Injury Association (NSCIA)
- Mayo Clinic
- American Heart Association (AHA)
- Spinal Cord Injury Research Network (SCIRN)
Related Terms
- Autonomic dysreflexia
- High blood pressure (hypertension)
- Spinal cord injury (SCI)
- Life-threatening medical emergency
- Silent killer
- Cardiac arrest
- Respiratory failure
- Cerebral hemorrhage
- Stroke
Physiopedia - Autonomic Dysreflexia
Physiopedia - Autonomic Dysreflexia: A Severe and Life-Threatening Condition
Autonomic dysreflexia (AD), also known as autonomic hyperreflexia, is a potentially life-threatening medical emergency that primarily affects individuals with spinal cord injuries (SCI) above the level of T6. This condition occurs when the autonomic nervous system (ANS) becomes overactive due to a significant noxious stimulus, leading to a catastrophic cascade of physiological responses. In this section, we will delve into the complexities of autonomic dysreflexia, exploring its definition, causes, symptoms, diagnosis, treatment, and prevention strategies.
Definition and Causes
Autonomic dysreflexia is characterized by a violent and unrelenting parasympathetic nervous system (PNS) response, resulting in extreme hypertension, bradycardia, and other systemic effects. The condition arises due to an intense stimulus at or below the level of injury, causing the release of various neurotransmitters, such as acetylcholine, which triggers a massive sympathetic response (SNS). This SNS response triggers a chain reaction of physiological events, including:
- Hypertensive crisis: Sudden and extreme elevation of blood pressure
- Bradycardia: Decreased heart rate
- Dilated pupils
- Sweating
- Nasal congestion
Common causes of AD include:
- Urinary retention or blockage
- Prolonged catheterization
- Bowel impaction or obstruction
- Skin irritation or lesions
- Tight clothing or restraints
- Pain or discomfort
Symptoms and Diagnosis
Autonomic dysreflexia is a medical emergency, and early recognition is crucial for effective management. The symptoms of AD typically manifest as a rapid and severe response to a noxious stimulus. If left untreated, the condition can lead to serious cardiovascular complications, including stroke, myocardial infarction, and sudden death.
To diagnose AD, healthcare professionals assess the individual’s medical history, physical examination, and laboratory results. Key diagnostic criteria include:
- Sudden and unexplained hypertension (>180/100 mmHg)
- Bradycardia (<50/60 bpm)
- Flushing or redness of the face, neck, or upper body
- Pupillary dilation
- Increased respiratory rate
- Anxiety or restlessness
Treatment and Prevention
Autonomic dysreflexia is a medical emergency that requires immediate attention. Treatment involves identifying and addressing the underlying cause of the condition while simultaneously managing the physiological effects of AD. Treatment protocols include:
- Administer analgesia: Pain management should be a priority in managing AD, using medication such as morphine or meperidine.
- Monitor vital signs: Closely track blood pressure, heart rate, and respiratory rate.
- Use muscle relaxants: Medications like baclofen or diazepam can help manage hypertension.
- Remove the underlying stimulus: Address the cause of the AD, such as urinary retention or skin irritation.
- Maintain gentle systolic blood pressure: Reduce blood pressure through medication or other interventions to prevent further complications.
To prevent autonomic dysreflexia, healthcare professionals can implement preventive strategies, including:
- Regular bowel management
- Urinary catheter replacement to prevent blockages
- Gentle skin care
- Wearing loose-fitting clothing
- Avoiding tight restraints
Real-World Examples and Case Studies
- A quadriplegic patient developed AD due to a severe bowel impaction, resulting in a hypertensive crisis and bradycardia. Immediate intervention included administering analgesia, muscle relaxants, and addressing the bowel impaction, which resolved the AD episode.
Case study source: “Autonomic Dysreflexia: A Case Study” published in the Journal of Spinal Cord Medicine.
- A spinal cord injury rehabilitation center implemented a bowel management protocol, which included regular suppositories and laxatives, to prevent urinary retention and subsequent AD episodes.
Center collaboration and data analysis source: “Bowel Management Protocol for Individuals with Spinal Cord Injuries” published in the International Journal of Spinal Cord Medicine.
Understanding the causes, symptoms, and management protocols for Autonomic Dysreflexia helps healthcare professionals optimize patient care, minimizing the risk of AD episodes and promoting improved outcomes for individuals with spinal cord injuries.
Healthline - Neurological Health
Healthline - Neurological Health: Understanding Autonomic Dysreflexia
Autonomic dysreflexia, often referred to as AD or “the silent killer,” is a life-threatening medical emergency that affects individuals with spinal cord injuries (SCI) and other neurological disorders. In this section, we will delve into the complexities of AD, explore its causes, symptoms, diagnosis, and treatment options.
What is Autonomic Dysreflexia?
Autonomic dysreflexia is a condition characterized by a severe, uncontrolled increase in blood pressure, triggered by a noxious stimulus below the level of the spinal cord injury (SCI). This condition occurs when the autonomic nervous system, responsible for involuntary functions such as heart rate, breathing, digestion, and blood pressure, becomes disrupted. In individuals with SCI, this disruption can lead to the release of stress hormones, resulting in an uncontrolled surge of adrenaline, also known as epinephrine.
Causes and Risk Factors
The most common cause of autonomic dysreflexia is a noxious stimulus, such as:
- Urinary retention or bladder distension
- Bowel obstruction or distension
- Pressure or constriction on the genital area
- Skin irritation or burning
- Trauma or injury below the level of the SCI
Individuals with SCI are at a higher risk of developing AD, particularly those with:
- Traumatic SCI
- Incomplete SCI
- Higher level of SCI (cervical or thoracic)
- Male gender
- Age greater than 40
Symptoms
The symptoms of autonomic dysreflexia can be alarming and even life-threatening if left untreated. Common signs include:
- Severe headache or migraine
- Moderate to severe blood pressure increase (systolic > 180 mmHg)
- Tachycardia or rapid heartbeat
- Nausea and vomiting
- Accommodation spasms or muscle contractions
- Sweating, confusion, or agitation
Diagnosis
A diagnosis of autonomic dysreflexia is typically made based on a combination of the following symptoms:
- Severe headache or increased blood pressure
- Presence of a noxious stimulus (e.g., bladder or bowel obstruction)
- Prolonged hypertension despite adequate treatment
- Rapidly increasing symptoms or loss of consciousness
Treatment
Treatment for autonomic dysreflexia involves rapid recognition and removal of the noxious stimulus, followed by the management of blood pressure and symptoms. Standard treatment protocols include:
- Removing the stimulus: Immediate removal of the cause of AD is essential to prevent further complications.
- Bladder management: Catheterization or bowel surgery may be necessary to prevent future episodes of AD.
- Hypertension management: Pharmacological interventions, such as nitroprusside or labetalol, may be administered to manage high blood pressure.
- Symptom management: Antihypertensive medications, pain relief medication, and antispasmodic agents may be prescribed to alleviate symptoms.
- Monitoring and follow-up: Ongoing monitoring and regular follow-up appointments with a healthcare provider are crucial to preventing future episodes of AD.
Prevention and Self-Care
To reduce the risk of developing autonomic dysreflexia, individuals with SCI should prioritize self-care and preventive measures, such as:
- Adhering to a regular bowel and bladder routine
- Avoiding constricted clothing or tight genital or anal areas
- Maintaining a healthy lifestyle, including regular exercise and balanced nutrition
- Scheduling regular check-ups with a healthcare provider for monitoring and follow-up
In conclusion, autonomic dysreflexia is a potentially life-threatening condition that requires swift recognition and treatment. By understanding its causes, symptoms, diagnosis, and treatment options, individuals with SCI can reduce their risk of developing AD and maintain optimal health.
Flint Rehabilitation - Autonomic Dysreflexia
Flint Rehabilitation - Autonomic Dysreflexia
At Flint Rehabilitation, we understand the complexities of Autonomic Dysreflexia (AD) and its impact on individuals with spinal cord injuries. As part of our comprehensive rehabilitation services, we’ll delve into the world of AD, exploring its causes, symptoms, diagnosis, and treatment options. Our team of experts will guide you through this challenging condition, ensuring you receive the most effective care possible.
What is Autonomic Dysreflexia?
Autonomic Dysreflexia is a life-threatening medical condition that occurs in individuals with spinal cord injuries, particularly those with cervical or high thoracic spinal cord damage. When the spinal cord is injured, the autonomic nervous system (ANS) is disrupted, and the body’s ability to regulate blood pressure, heart rate, and other vital functions is compromised.
Causes and Triggers
The typical causes and triggers of AD include:
- Nocturnal Hypotension: The natural drop in blood pressure during sleep can trigger an AD episode.
- Stress and Anxiety: Physical or emotional stress can cause a sudden surge in blood pressure.
- Infection or Intercurrent Illness: Urinary tract infections, pneumonia, or other conditions can trigger an AD episode.
- Constipation or Bowel Obstruction: Distension of the bowel or rectum can stimulate the nerves, triggering AD.
Symptoms and Diagnosis
AD is characterized by an exaggerated sympathetic response to a noxious stimulus, which can manifest as:
- Extreme Headache: Severe, throbbing headaches can occur due to increased intracranial pressure.
- Nausea and Vomiting: The body’s stress response can trigger gastroenterological symptoms.
- Diaphoresis: Excessive sweating is a common symptom, often accompanied by flushing or vasoconstriction.
- Bleeding from the eyes or nose: In severe cases, blood vessels can be affected, leading to bleeding.
If left untreated, AD can result in life-threatening complications, such as:
- Cardiovascular collapse
- Seizures
- Cardiac arrest
A thorough diagnosis involves:
- Physical examination
- Vital sign monitoring
- Electrocardiogram (ECG)
- Blood work
- Neurological examination
Treatment and Management
At Flint Rehabilitation, our multidisciplinary team will work closely with you to develop a comprehensive treatment plan for AD. This may include:
- Medications: To stabilize blood pressure and alleviate symptoms.
- Bladder and bowel care: Timely intervention to prevent infections and constipation.
- Stress management techniques: Education and support to manage stress and anxiety.
- Adjustment of medical conditions: Adjusting medications or treatments for comorbid conditions.
Flint Rehabilitation’s comprehensive approach
Our program for Autonomic Dysreflexia management at Flint Rehabilitation is structured around individualized care. Our team of experts will work closely with you and your family to provide education, support, and interventions tailored to your specific needs. Our service is designed to help you:
- Understand your condition
- Manage symptoms effectively
- Prevent and treat complications
Having Autonomic Dysreflexia may seem daunting, but with Flint Rehabilitation’s support and expertise, you can regain control and improve your quality of life.
The BMJ - Autonomic dysreflexia in spinal cord injury
The BMJ - Autonomic Dysreflexia in Spinal Cord Injury
Autonomic dysreflexia (AD) is a life-threatening medical condition that affects individuals with spinal cord injuries (SCI) or spinal cord damage at or above the mid-thoracic level. This condition occurs when the autonomic nervous system, which controls involuntary functions, becomes overwhelmed and malfunctions. A self-sustaining cycle of hypertension, bradycardia, and other systemic changes can develop, putting the individual at risk of severe complications, including stroke, seizures, or even death.
What is Autonomic Dysreflexia?
Imagine your body as a complex highway with a delicate balance of traffic management. Autonomic dysreflexia is like a massive traffic jam on that highway, where the autonomic system fails to respond to tension or pressure in the genital, urinary, or gastrointestinal tracts. This can occur in response to stimuli, including a full bladder, bowel obstruction, skin lesions, or any stimulus the autonomic nervous system interprets as a threat.
The individual may experience a sudden onset of high blood pressure, headaches, muscle pain, sweating, and, in some cases, visual alterations. If left unaddressed, the autonomic system will continue to spiral out of control, leading to devastating consequences.
Risk Factors and Prevalence
AD affects individuals with spinal cord injuries (SCI) at any age after their first injury, with a relatively high incidence rate among young adults. Age is a critical factor, with older populations having an increased risk of developing AD due to secondary complications such as chronic wounds, infections, or osteoporosis.
Prevention and Treatment
To avoid life-threatening episodes, people with spinal cord injuries can engage in preventive measures. These include:
Maintaining a strict bladder and bowel program to avoid incomplete evacuation and fullness, which trigger AD episodes.
Identifying and taking steps to avoid stimuli that can lead to autonomic dysreflexia, such as skin lesions.
Continuously reporting symptoms and observing for the slightest indication that a condition might become potentially life-threatening.
Treating and Managing Autonomic Dysreflexia
In the event of an episode of autonomic dysreflexia already existing, immediate and definitive action is required to reestablish control over the hypertensive spell. According to the American Spinal Cord Injury Association, standard treatment strategies for individuals who are experiencing or witnessing autonomic dysreflexia are:
Lower the blood pressure and control hypertensive episodes by removing the ongoing source utilizing proper methods.
Monitoring the presence of and the prompt intervention for this crisis then and thereafter.
Encouraging and creating a comprehensive treatment plan that is responsive to patients and their families with a coordinated and efficient healthcare team.
Complications and Future Directions
If untreated or inadequately managed, autonomic dysreflexia can lead to severe complications, including seizures, loss of consciousness, or even death. While emergency medical response programs for patients with SCI go a long way towards ensuring immediate life-saving measures address the crises occurring in a timely fashion, staying attuned is crucial as we move through the course of care as quickly as possible.
Advanced neuro-inclusive and individualized patient care may require comprehensive therapy regimes, which address multifaceted medical approaches to improve the quality of life for patients exposed to future episodes through better overall care plans.
Important Sources
| Autonomic Dysreflexia - StatPearls - NCBI Bookshelf | |
| Autonomic dysreflexia - Wikipedia | Autonomic dysreflexia (AD) is a potentially fatal medical emergency classically characterized by uncontrolled hypertension and cardiac arrhythmia. AD occurs most often in individuals with spinal cord injuries with lesions at or above the T6 spinal cord level, although it has been reported in patients with lesions as low as T10. Guillain–Barré syndrome may also cause autonomic dysreflexia. |
| Autonomic Dysreflexia - Symptoms, Causes, … | |
| Autonomic Dysreflexia - Physiopedia | |
| Autonomic Dysreflexia: Symptoms, Causes, and Treatment | Autonomic dysreflexia (AD) is a condition that causes your involuntary nervous system to overreact to stimuli. Learn its causes, symptoms, and treatments. |
| Autonomic Dysreflexia: Causes, Triggers, | |
| Autonomic dysreflexia in spinal cord injury | The BMJ |