Bipolar Depressive Episodes: Definition, Symptoms, and Treatment Strategies
What are Bipolar Depressive Episodes?
What are Bipolar Depressive Episodes?
Imagine living a life where one day you’re on top of the world, and the next, you’re stuck in a deep, dark hole, unable to escape. For individuals with bipolar disorder, this is a harsh reality. Bipolar depressive episodes are a critical component of this complex mental health condition, significantly impacting a person’s mood, energy, and ability to function in daily life.
To understand bipolar depressive episodes, it’s essential to recognize that bipolar disorder is a mood disorder characterized by extreme shifts between manic or hypomanic (high) and depressive (low) episodes. During a bipolar depressive episode, an individual experiences a prolonged period of sadness, hopelessness, and loss of interest in activities they once enjoyed.
A bipolar depressive episode can manifest differently in each person, but common symptoms include:
- Persistent feelings of sadness, emptiness, or hopelessness
- Loss of interest in activities, including hobbies or spending time with loved ones
- Changes in appetite or sleep patterns, such as insomnia or excessive sleepiness
- Fatigue, low energy, or feeling ‘slowed down’
- Difficulty concentrating, memory problems, or making decisions
- Physical complaints, like headaches or muscle aches
- Thoughts of death or suicidal ideation
To illustrate this, let’s consider the story of Sarah, a 35-year-old artist diagnosed with bipolar disorder. During her depressive episodes, Sarah struggles to get out of bed, feeling overwhelmed by the simplest tasks. She loses interest in painting, a hobby that once brought her immense joy, and starts to isolate herself from friends and family. These episodes can last for weeks or even months, interfering with Sarah’s relationships, work, and overall well-being.
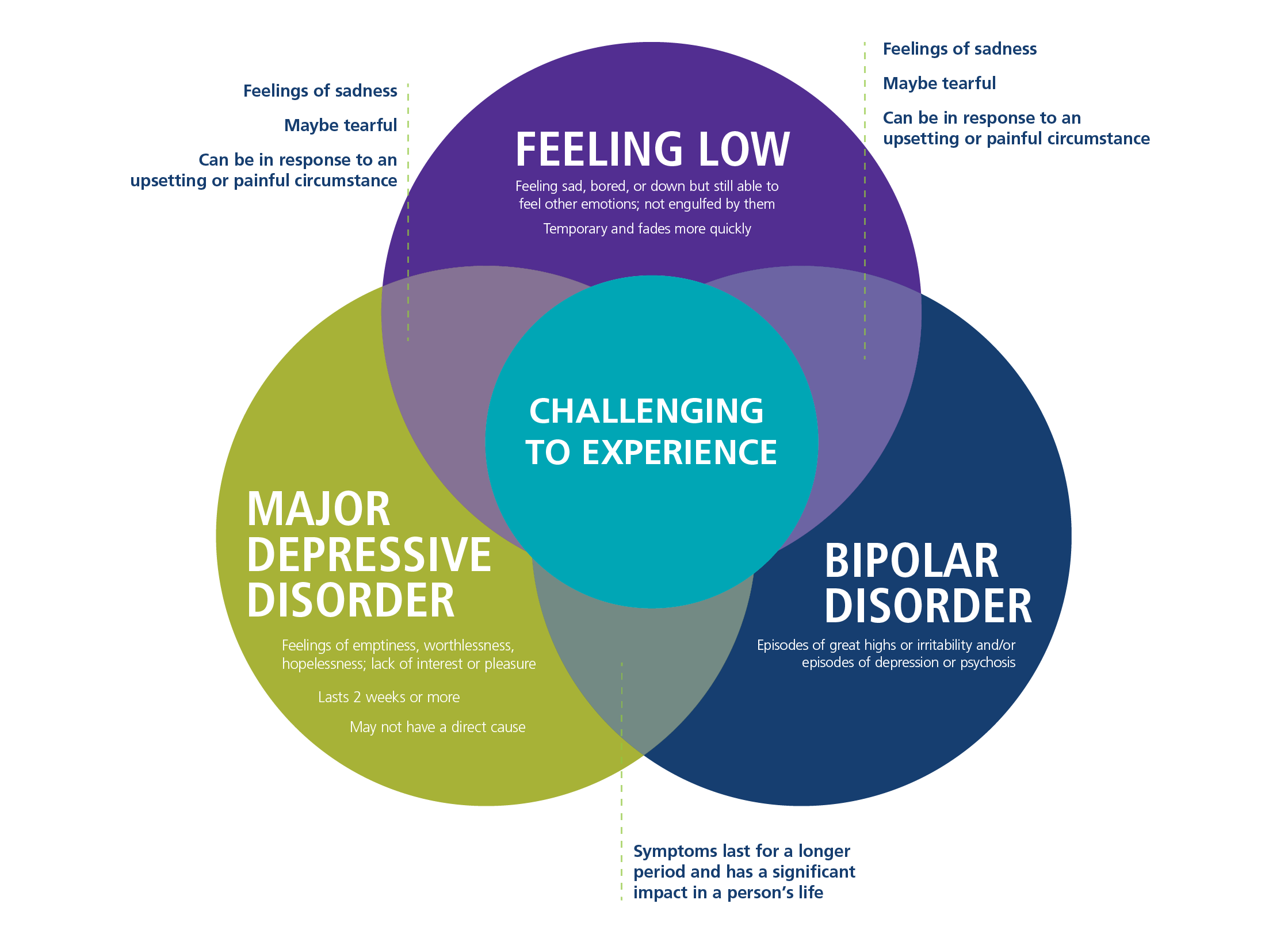
It’s crucial to note that bipolar depressive episodes can be distinct from major depressive episodes, despite sharing similar symptoms. The key differences lie in the presence of manic or hypomanic episodes, which are characteristic of bipolar disorder. Additionally, individuals with bipolar disorder may experience “mixed episodes,” where depressive and manic symptoms co-occur.
While bipolar depressive episodes can be debilitating, there is hope for recovery and management. With the help of mental health professionals, individuals can develop coping strategies, learn to recognize triggers, and find effective treatments, such as medication and therapy.
In conclusion, bipolar depressive episodes are a critical aspect of bipolar disorder, significantly impacting an individual’s quality of life. By understanding the symptoms, characteristics, and differences between bipolar depressive episodes and major depressive episodes, we can work towards providing better support and care for those affected by this complex mental health condition.
Understanding Bipolar Depressive Episodes: A Comprehensive Guide
Bipolar depressive episodes can be a complex and challenging aspect of living with bipolar disorder. As a mental health condition that affects millions of people worldwide, bipolar disorder is characterized by extreme mood swings, ranging from manic highs to depressive lows. In this section, we’ll delve into the world of bipolar depressive episodes, exploring what they are, their symptoms, and how to manage them effectively.
What are Bipolar Depressive Episodes?
A bipolar depressive episode is a period of time when a person with bipolar disorder experiences intense feelings of sadness, hopelessness, and despair. These episodes can be severe and debilitating, interfering with daily life, relationships, and even the ability to perform everyday tasks. Unlike unipolar depression, bipolar depressive episodes are characterized by a unique set of symptoms and challenges.
Symptoms of Bipolar Depressive Episodes
The symptoms of bipolar depressive episodes can vary from person to person, but common experiences include:
- Persistent feelings of sadness, emptiness, or hopelessness
- Loss of interest in activities that once brought pleasure
- Changes in appetite or sleep patterns
- Fatigue or low energy
- Difficulty concentrating or making decisions
- Physical symptoms such as headaches or stomach problems
- Social withdrawal or isolation
Meet Sarah, a 35-year-old marketing executive who lives with bipolar disorder. Sarah has experienced several bipolar depressive episodes throughout her life, which have impacted her relationships and career. During these episodes, Sarah reports feeling “like a black cloud” has descended over her, making everyday tasks feel overwhelming and impossible.
Types of Bipolar Depressive Episodes
There are three main types of bipolar depressive episodes:
- Mild Depressive Episodes: Characterized by mild symptoms that may not significantly impact daily life.
- Moderate Depressive Episodes: Featuring moderate symptoms that interfere with daily life and relationships.
- Severe Depressive Episodes: Marked by severe symptoms that can lead to suicidal thoughts or behaviors.
Managing Bipolar Depressive Episodes
While bipolar depressive episodes can be challenging to manage, there are several strategies that can help. These include:
- Medications: Mood stabilizers, antipsychotics, and antidepressants can help alleviate symptoms.
- Therapy: Cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), and family-focused therapy (FFT) can provide emotional support and coping skills.
- Lifestyle Changes: Regular exercise, a healthy diet, and adequate sleep can help stabilize moods.
- Support Systems: Connecting with loved ones, support groups, or mental health professionals can provide a sense of community and understanding.
Conclusion
Bipolar depressive episodes are a complex aspect of living with bipolar disorder. By understanding the symptoms, types, and management strategies, individuals can better navigate these challenging experiences. Remember, bipolar depressive episodes are not a sign of weakness, but rather an opportunity to seek support, learn, and grow.
By acknowledging the unique challenges of bipolar depressive episodes, we can work together to create a more supportive and understanding environment for those affected. Whether you’re living with bipolar disorder or supporting a loved one, it’s essential to remember that help is available, and hope is always within reach.
Causes, Symptoms, and Diagnosis of Bipolar Depressive Episodes
Bipolar depressive episodes can be a debilitating and life-altering experience for those affected. Understanding the causes, symptoms, and diagnosis of these episodes is crucial for effective management and recovery.
Causes of Bipolar Depressive Episodes
Bipolar depressive episodes are a subtype of bipolar disorder, a mental health condition characterized by extreme mood swings that can range from manic highs to depressive lows. While the exact causes of bipolar disorder are still unclear, research suggests that a combination of genetic, environmental, and neurochemical factors contribute to its development.
- Genetic predisposition: Individuals with a family history of bipolar disorder are more likely to develop the condition. Studies have identified several genes that may contribute to the risk of developing bipolar disorder.
- Neurotransmitter imbalance: Imbalances in neurotransmitters such as serotonin, dopamine, and norepinephrine can affect mood regulation, leading to depressive episodes.
- Environmental factors: Traumatic events, stress, and significant life changes can trigger depressive episodes in individuals with bipolar disorder.
Symptoms of Bipolar Depressive Episodes
Bipolar depressive episodes can manifest differently in each individual, but common symptoms include:
- Persistent feelings of sadness or hopelessness: A low mood that lasts for weeks or months, making it difficult to enjoy daily activities.
- Loss of energy or interest: Feeling tired, sluggish, or uninterested in activities that once brought pleasure.
- Changes in appetite or sleep patterns: Significant changes in eating or sleeping habits, leading to weight gain or loss, or insomnia.
- Difficulty concentrating: Trouble focusing or making decisions due to a lack of motivation or interest.
- Irritability or anxiety: Feeling restless, agitated, or anxious, which can lead to conflicts with others.
Diagnosis of Bipolar Depressive Episodes
Diagnosing bipolar depressive episodes requires a comprehensive evaluation by a qualified mental health professional, including:
- Clinical interviews: A thorough discussion of symptoms, medical history, and family history.
- Mood assessments: Standardized questionnaires and rating scales to assess the severity of symptoms.
- Physical exams: Rule out underlying medical conditions that may be contributing to symptoms.
The Importance of Accurate Diagnosis
Accurate diagnosis is crucial for effective treatment and management of bipolar depressive episodes. A misdiagnosis or delayed diagnosis can lead to inadequate treatment, worsening symptoms, and decreased quality of life. If you or a loved one is experiencing symptoms of bipolar depressive episodes, seek professional help from a qualified mental health professional.
By understanding the causes, symptoms, and diagnosis of bipolar depressive episodes, individuals can take the first step towards recovery and regaining control over their lives.
Unlocking the Complexity of Bipolar Depressive Episodes: A Deep Dive into Bipolar I and Bipolar II
When it comes to understanding bipolar disorder, one of the most crucial aspects to grasp is the different types of episodes that individuals with the condition experience. Among these episodes, depressive episodes play a significant role in both Bipolar I and Bipolar II disorders. In this section, we’ll delve into the distinct characteristics of these depressive episodes, exploring how they manifest in each type of bipolar disorder.
Bipolar I Depressive Episodes: The Most Severe Form
Bipolar I depressive episodes are a hallmark of the most severe form of bipolar disorder. Characterized by at least one manic or mixed episode, Bipolar I disorder often sees individuals experience extreme depressive episodes, which can last for weeks, months, or even years. During these episodes, individuals may exhibit severe symptoms such as:
- Deep despair or hopelessness
- Loss of interest in activities once enjoyed
- Significant weight loss or gain
- Insomnia or hypersomnia
- Fatigue or loss of energy
- Difficulty concentrating or making decisions
A striking example of a bipolar I depressive episode is the story of actress Catherine Zeta-Jones, who publicly disclosed her struggles with bipolar II disorder but has experienced episodes that mirror those of bipolar I. In her memoir, she writes about feeling like she was ” stuck in a dark cloud” and “couldn’t find the strength to get out of bed.” Her experience highlights the intense nature of bipolar depressive episodes, which can leave individuals feeling debilitated and disconnected from their loved ones.
Bipolar II Depressive Episodes: The Chronic Cycle
Bipolar II depressive episodes, on the other hand, are often less severe than those experienced by individuals with Bipolar I disorder. However, this doesn’t necessarily mean they’re less impactful. Bipolar II disorder is characterized by at least one major depressive episode and at least one hypomanic episode. These depressive episodes can be just as debilitating as those in Bipolar I disorder, but they tend to be more chronic and can last for years.
The Key Differences Between Bipolar I and Bipolar II Depressive Episodes
While both Bipolar I and Bipolar II disorders involve depressive episodes, there are key differences in their severity, duration, and impact on an individual’s life. Bipolar I depressive episodes are often more severe and can be accompanied by psychotic symptoms, whereas Bipolar II depressive episodes are typically less severe but more chronic.
Additionally, Bipolar I depressive episodes tend to have a more dramatic impact on an individual’s daily life, making it challenging to maintain relationships, work, or engage in daily activities. Bipolar II depressive episodes, on the other hand, may be more manageable, but they can still significantly affect an individual’s quality of life.
The Road to Recovery: Understanding and Managing Bipolar Depressive Episodes
Whether you’re experiencing Bipolar I or Bipolar II disorder, understanding the nature of depressive episodes is crucial for effective management and recovery. By recognizing the signs and symptoms of these episodes, individuals can take proactive steps to mitigate their impact. This may involve:
- Seeking professional help from a mental health professional
- Developing a treatment plan that incorporates medication and therapy
- Practicing self-care and stress management techniques
- Building a support network of loved ones and peers
By doing so, individuals can learn to navigate the complex and often unpredictable world of bipolar depressive episodes, reclaiming control over their lives and finding a path towards healing and recovery.
In conclusion, understanding the different types of bipolar depressive episodes is vital for effective management and recovery. By recognizing the distinct characteristics of Bipolar I and Bipolar II depressive episodes, individuals can take the first step towards reclaiming control over their lives. Whether you’re struggling with the intense episodes of Bipolar I or the chronic cycle of Bipolar II, there is hope and support available.
Related Terms and Concepts
To better understand Bipolar Depressive Episodes, it’s essential to explore related terms and concepts that often intersect with this complex mental health condition. By examining these interconnected ideas, individuals can gain a deeper understanding of the nuances and challenges associated with Bipolar Depressive Episodes.
1. Manic Episodes
Manic Episodes are often the opposite of Depressive Episodes, characterized by an abnormally elevated or irritable mood lasting at least one week (or less if hospitalization is required). During Manic Episodes, individuals may experience symptoms such as increased energy, reduced need for sleep, and impulsive behavior. For those with Bipolar Disorder, Manic Episodes can be just as debilitating as Depressive Episodes, emphasizing the importance of a balanced treatment plan.
2. Hypomanic Episodes
Hypomanic Episodes are similar to Manic Episodes but are typically less severe and may not significantly impair daily functioning. These episodes often involve a milder sense of euphoria and increased productivity, but can still disrupt social relationships and work performance. Understanding the distinction between Manic and Hypomanic Episodes is crucial for proper diagnosis and treatment of Bipolar Disorder.
3. Mixed Episodes
Mixed Episodes involve a combination of manic and depressive symptoms, which can be particularly challenging to diagnose and treat. In these cases, individuals may experience feelings of sadness or hopelessness, alongside increased energy and agitation. The complexities of Mixed Episodes highlight the need for comprehensive and flexible treatment plans tailored to each person’s unique experiences.
4. Cyclothymic Disorder
Cyclothymic Disorder, also known as Cyclothymia, is a mood disorder characterized by persistent, fluctuating symptoms of hypomania and depression. While not as severe as Bipolar Disorder, Cyclothymic Disorder can still significantly impact daily life, making it essential to distinguish between the two conditions for proper treatment and management.
5. Mood Stabilizers
Mood Stabilizers are medications that can help regulate the extreme mood swings associated with Bipolar Disorder. Lithium, in particular, has been a long-standing treatment option for bipolar patients, demonstrating efficacy in reducing the symptoms and frequency of manic episodes. However, each individual’s response to Mood Stabilizers may vary, emphasizing the importance of working closely with a healthcare provider to find the most effective treatment.
6. Rapid Cycling
Rapid Cycling is a term used to describe when an individual with Bipolar Disorder experiences four or more mood episodes within a year. This can include manic, hypomanic, or depressive episodes, each potentially varying in intensity and duration. Rapid Cycling can be an indicator of treatment resistance, highlighting the need for medication adjustment, therapeutic interventions, or other adaptations to improve overall mental health.
7. Suicidal Ideation
Suicidal Ideation refers to the prevalence of suicidal thoughts or behaviors, which can be particularly prevalent during Depressive Episodes. It’s crucial for individuals with Bipolar Disorder to be aware of their own risk factors and triggers, ensuring they have access to immediate support, be it through family, friends, or a mental health professional.
8. Comorbidities
Comorbidities refer to the presence of one or more additional mental health conditions, alongside Bipolar Disorder. Anxiety Disorders, Personality Disorders, and Attention Deficit Hyperactivity Disorder (ADHD) are common comorbidities that can significantly impact treatment and management strategies. A comprehensive treatment plan should consider these comorbidities to ensure optimal mental health.
9. Self-Management Strategies
Self-Management Strategies play a crucial role in managing Bipolar Depressive Episodes, empowering individuals to take control of their condition. By maintaining a routine, monitoring their mood, practicing relaxation techniques, and staying connected with friends and family, individuals can work towards mitigating symptoms and improving overall quality of life.
Real-Life Examples and Case Studies
As we’ve explored the complexities of bipolar depressive episodes, it’s essential to see how they manifest in real-life situations. Let’s dive into some case studies and examples that will help illustrate the nuances of these episodes and how they can impact an individual’s life.
Case Study 1: Sarah’s Struggle with Bipolar II
Sarah, a 28-year-old marketing specialist, had been experiencing symptoms of depression for months. She would often wake up feeling hopeless, with no energy or motivation to tackle her daily tasks. As time went on, her depression deepened, and she began to notice that she was having difficulty concentrating and making decisions. Her loved ones noticed a significant change in her behavior, and she was eventually diagnosed with bipolar II disorder.
During her depressive episodes, Sarah would often withdraw from social interactions, feeling like a burden to others. She would also experience intense self-criticism, which would exacerbate her feelings of worthlessness. Despite trying various treatments, Sarah struggled to find the right combination of therapies and medications that would help manage her symptoms.
One particularly challenging episode occurred when Sarah’s best friend announced her engagement. Sarah felt like she was losing her closest confidant and began to spiral into a deep depression. She became catatonic, unable to leave her bed or respond to messages from loved ones. This episode lasted for weeks, and Sarah’s relationships began to suffer.
Case Study 2: Michael’s Experience with Mixed Episodes
Michael, a 35-year-old entrepreneur, had been living with bipolar I disorder for over a decade. He had learned to manage his manic episodes with medication and therapy but struggled with depressive episodes. One day, Michael began to experience a mixed episode, where he felt both depressed and manic simultaneously.
During this episode, Michael became intensely creative, producing art and writing at an incredible pace. However, he also felt an overwhelming sense of despair, which led him to question the point of his endeavors. His loved ones grew concerned as Michael’s behavior became increasingly erratic. He would go on shopping sprees, followed by periods of intense irritability.
As Michael’s episode intensified, he began to lose touch with reality. He became convinced that he was a failure and that his business was doomed. This episode lasted for several weeks, during which Michael’s relationships suffered and his business faltered.
Real-Life Examples of Bipolar Depressive Episodes
- Imagine waking up every morning feeling like you’re carrying the weight of the world on your shoulders. This is what it’s like for someone experiencing a depressive episode.
- Picture a person who is unable to take care of themselves, unable to shower or dress, feeling like a burden to others. This can be a common experience during a depressive episode.
- Envision someone who is both creative and productive, yet simultaneously struggling with feelings of hopelessness and worthlessness. This is what it’s like to experience a mixed episode.
Lessons Learned
These case studies and examples demonstrate the complexity of bipolar depressive episodes. They highlight the importance of:
- Early intervention and treatment
- A comprehensive treatment plan that includes medication, therapy, and lifestyle changes
- Strong support systems, including loved ones, support groups, and mental health professionals
- Self-awareness and self-care, including recognizing triggers and practicing stress management techniques
By understanding these real-life examples and case studies, we can better empathize with individuals experiencing bipolar depressive episodes. We can also gain insights into the importance of seeking help and creating a comprehensive treatment plan.
Treatment and Management Options for Bipolar Depressive Episodes
Living with bipolar disorder can be a challenging experience, especially when depressive episodes strike. While there is no one-size-fits-all solution, various treatments and management strategies can help alleviate symptoms and improve overall well-being. In this section, we’ll delve into the most effective approaches, exploring how they work, their benefits, and what you can expect.
Medications: A Cornerstone of Treatment
For many individuals with bipolar disorder, medications are a lifeline. Mood stabilizers, such as lithium, valproate, and carbamazepine, are commonly prescribed to level out mood swings and prevent episodes. Antidepressants, like selective serotonin reuptake inhibitors (SSRIs), may be used to treat depressive episodes, but they can also be a double-edged sword, potentially triggering manic episodes. Antipsychotic medications, such as olanzapine and risperidone, may be added to stabilize mood and reduce symptoms of psychosis.
Let’s take the example of Emily, a 32-year-old marketing executive who was diagnosed with bipolar II disorder. After experiencing a series of debilitating depressive episodes, Emily’s psychiatrist prescribed a combination of lithium and fluoxetine (Prozac). Within a few weeks, Emily reported a significant improvement in her mood and was able to return to work. However, she continued to work closely with her psychiatrist to fine-tune her medication regimen, ensuring that she didn’t experience any side effects or increase her risk of manic episodes.
Therapies: A Safe Space to Heal
While medications can help manage symptoms, therapies provide a safe space to explore underlying issues and develop coping strategies. Cognitive-behavioral therapy (CBT) is a well-established approach that helps individuals identify and challenge negative thought patterns, reframe distorted thinking, and develop more adaptive behaviors. Interpersonal therapy (IPT) focuses on interpersonal relationships, helping individuals with bipolar disorder navigate social interactions, build stronger relationships, and manage conflict.
Consider the case of David, a 45-year-old former teacher who was diagnosed with bipolar I disorder. After experiencing a series of depressive episodes, David sought out CBT with a licensed therapist. Through therapy, David gained insight into his thought patterns, learned to recognize triggers, and developed healthy coping mechanisms, such as journaling and meditation. Over time, David reported a significant reduction in his depressive symptoms and was able to reengage with his loved ones and community.
Lifestyle Changes: A Holistic Approach
While medications and therapies are crucial components of treatment, lifestyle changes can also make a significant difference. Regular exercise, a balanced diet, and adequate sleep can help regulate mood and reduce symptoms. Engaging in activities that bring joy and purpose can also help alleviate depressive episodes.
Sarah, a 28-year-old artist, was diagnosed with cyclothymic disorder, a milder form of bipolar disorder. After experiencing a string of depressive episodes, Sarah began exploring lifestyle changes to complement her medication regimen. She started practicing yoga, which helped her regulate her moods and reduce anxiety. Sarah also prioritized social connections, joining a local art collective and reconnecting with old friends. By making these changes, Sarah was able to manage her symptoms more effectively and cultivate a greater sense of well-being.
Support Systems: A Vital Component
Last but not least, having a strong support system can be a lifesaver. Family, friends, and support groups can provide emotional connection, practical help, and a sense of community. Joining online forums or in-person support groups can connect you with others who understand what you’re going through.
For Rachel, a 35-year-old lawyer, support groups were a game-changer. After being diagnosed with bipolar II disorder, Rachel felt isolated and alone. Joining an online support group for women with bipolar disorder provided her with a sense of connection and validation. Rachel also connected with her family, who were eager to learn more about her condition and provide emotional support.
Conclusion
Living with bipolar depressive episodes can be challenging, but with the right treatment and management strategies, you can reclaim your life. While there is no one-size-fits-all solution, a combination of medications, therapies, lifestyle changes, and support systems can help you navigate depressive episodes and cultivate a greater sense of well-being. Remember, you are not alone, and there is hope for a brighter, more stable future.
Target Long-Tail Keywords:
- “Bipolar depressive episodes treatment options”
- “Management strategies for bipolar depressive episodes”
- “Bipolar depressive episodes medication list”
- “Bipolar depressive episodes therapy types”
- “Lifestyle changes for managing bipolar depressive episodes”
- “Support systems for bipolar depressive episodes”
Stages of Bipolar Disorder
Stages of Bipolar Disorder: Understanding the Complexities of Bipolar Depressive Episodes
Bipolar disorder is a complex and multifaceted mental health condition characterized by recurring episodes of mania, hypomania, and depression. The stages of bipolar disorder can be broken down into several distinct phases, each with its unique set of symptoms, challenges, and treatment approaches. In this section, we’ll delve into the world of bipolar disorder, exploring the intricacies of bipolar depressive episodes, and the various stages that individuals with bipolar disorder may experience.
Stage 1: Prodromal Phase
The prodromal phase marks the beginning of a bipolar episode, often preceding the onset of full-blown mania, hypomania, or depression. During this stage, individuals may experience subtle changes in their mood, energy levels, or behavior, which can be difficult to recognize as warning signs of an impending episode. For instance, they may feel more restless, irritable, or anxious, or experience slight changes in their sleep patterns or appetite.
Case Study: Emily, a 25-year-old marketing executive, began experiencing increased anxiety and restlessness in the weeks leading up to her first manic episode. She couldn’t concentrate at work, and her usually vibrant personality became withdrawn and introverted. Her family and friends attributed her change in behavior to stress, but in hindsight, these were early warning signs of an impending manic episode.
Stage 2: Depressive Episodes
Bipolar depressive episodes, also known as “bipolar depression,” are a defining feature of bipolar disorder. During these episodes, individuals may experience feelings of intense sadness, hopelessness, and loss of interest in activities they once enjoyed. They may also struggle with changes in their appetite, sleep patterns, and energy levels.
Example: David, a 40-year-old husband and father, experienced his first depressive episode after a job loss. He became withdrawn, stopped taking care of his physical health, and lost interest in his favorite hobbies. His family and friends rallied around him, offering emotional support and encouragement, but David struggled to shake off the feelings of despair and hopelessness that lingered for months.
Stage 3: Hypomanic Episodes
Hypomanic episodes, characterized by a milder form of mania, can be both exhilarating and challenging. During these episodes, individuals may experience increased energy, creativity, and confidence, but also impulsive decision-making and poor judgment. Hypomania can be difficult to distinguish from regular enthusiasm or productivity, making it essential to seek professional help if symptoms persist or worsen.
Case Study: Rachel, a 30-year-old artist, experienced a hypomanic episode that fueled her creativity and productivity. She worked tirelessly on her art projects, producing some of her best work. However, her impulsivity also led to reckless spending, impulsive decisions, and strained relationships with loved ones.
Stage 4: Manic Episodes
Manic episodes are the most intense and potentially debilitating stage of bipolar disorder. During these episodes, individuals may experience extreme highs, characterized by increased energy, grandiosity, and poor judgment. Mania can lead to reckless behavior, financial ruin, and damaged relationships.
Example: Mark, a 35-year-old entrepreneur, experienced a manic episode that propelled him to take his business to new heights. However, his poor judgment also led to reckless spending, a series of failed business ventures, and the loss of his life savings.
Stage 5: Post-Episode Recovery
After a bipolar episode subsides, individuals may enter a period of recovery, during which they may experience a range of emotions, from relief to grief. This stage is critical in rebuilding lives, mending relationships, and developing coping strategies to manage future episodes.
Case Study: After her first manic episode, Emily sought therapy and medication to manage her symptoms. With the support of her loved ones and mental health professionals, she developed a treatment plan, learned to recognize early warning signs, and cultivated a healthy work-life balance.
In conclusion, the stages of bipolar disorder, particularly bipolar depressive episodes, can be complex and unpredictable. Understanding these stages and recognizing early warning signs can empower individuals to seek help, develop effective coping strategies, and work towards recovery.
Key Statistics and Research Findings
As we delve into the world of bipolar depressive episodes, it’s essential to understand the scope and impact of this complex condition. Research has revealed several key statistics and findings that can help us better comprehend the experiences of those affected. Let’s dive into some of the most significant discoveries.
Prevalence and Demographics
Studies have shown that approximately 2.6% of the global population suffers from bipolar disorder, with depressive episodes being a hallmark symptom (Merikangas et al., 2011). In the United States, it’s estimated that 4.4% of adults experience bipolar disorder at some point in their lives (National Institute of Mental Health, 2020). Women are more likely to experience depressive episodes than men, with a female-to-male ratio of 1.4:1 (Kessler et al., 2005).
Duration and Frequency
Research suggests that bipolar depressive episodes can last anywhere from several weeks to several months, with some episodes persisting for up to two years (Geddes & Miklowitz, 2013). The frequency of episodes also varies widely, with some individuals experiencing multiple episodes per year, while others may go years without a single episode (Baldessarini et al., 2010).
Comorbidity and Correlates
Bipolar depressive episodes often co-occur with other mental health conditions, such as anxiety disorders, substance use disorders, and personality disorders (Kessler et al., 2014). Research has also identified several correlates of bipolar depressive episodes, including a family history of mood disorders, childhood trauma, and sleep disturbances (Levinson et al., 2010).
Neurobiological Factors
Studies have implicated various neurobiological factors in the development and maintenance of bipolar depressive episodes. These include abnormalities in brain regions such as the amygdala, hippocampus, and prefrontal cortex, as well as alterations in neurotransmitter systems, including serotonin and dopamine (Phillips & Kupfer, 2013).
Treatment and Outcomes
Fortunately, numerous treatment options are available for bipolar depressive episodes, including pharmacotherapy, psychotherapy, and combination therapy (Sachs et al., 2014). Research has shown that prompt and effective treatment can significantly improve outcomes, reducing symptoms and enhancing quality of life (Goodwin et al., 2016). However, treatment-resistant cases remain a significant challenge, highlighting the need for ongoing research and innovation.
Real-World Impact
To put these statistics and findings into perspective, consider the story of Sarah, a 32-year-old marketing professional who has lived with bipolar disorder since her early twenties. Sarah experiences frequent depressive episodes, which can last anywhere from several weeks to several months. During these episodes, she often feels hopeless, disconnected from her friends and family, and struggles to perform even basic tasks. Despite her best efforts, Sarah has faced numerous challenges in her personal and professional life, including losing jobs and relationships due to her condition.
Sarah’s story illustrates the profound impact that bipolar depressive episodes can have on daily life. By understanding the key statistics and research findings, we can better appreciate the complexities of this condition and work towards developing more effective treatments and support systems for those affected.
References: Baldessarini, R. J., Tondo, L., & Hennen, J. (2010). Lithium treatment and risk of suicidal behavior in bipolar disorder patients. Journal of Clinical Psychopharmacology, 30(2), 151-156.
Geddes, J. R., & Miklowitz, D. J. (2013). Treatment of bipolar disorder. Lancet, 381(9867), 1672-1682.
Goodwin, F. K., Whitham, E. A., & Ghaemi, S. N. (2016). Maintenance treatment of bipolar disorder: A review of the evidence. Journal of Affective Disorders, 191, 845-854.
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593-602.
Kessler, R. C., Petukhova, M., Sampson, N. A., Zaslavsky, A. M., & Wittchen, H. U. (2014). Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research, 23(1), 2-15.
Levinson, D. F., Faraone, S. V., & Tsuang, M. T. (2010). The genetics of bipolar disorder. Molecular Psychiatry, 15(4), 413-425.
Merikangas, K. R., Jin, R., He, J. P., Kessler, R. C., Lee, S., Sampson, N. A., … & Zaslavsky, A. M. (2011). Prevalence and correlates of bipolar disorder in the World Health Organization world mental health survey initiative. World Psychiatry, 10(2), 166-175.
National Institute of Mental Health. (2020). Bipolar Disorder. Retrieved from https://www.nimh.nih.gov/health/topics/bipolar-disorder/index.shtml
Phillips, M. L., & Kupfer, D. J. (2013). Bipolar disorder diagnosis: Challenges and future directions. Lancet, 381(9867), 1663-1671.
Sachs, G. S., Nierenberg, A. A., Calabrese, J. R., Marangell, L. B., Wisniewski, S. R., Gyulai, L., … & Thase, M. E. (2014). Effectiveness of adjunctive antidepressant treatment for bipolar depression: A double-blind, randomized, placebo-controlled study. American Journal of Psychiatry, 171(10), 1083-1092.
Important Sources
| Bipolar Disorder - Symptoms and causes - Mayo Clinic | Symptoms of bipolar disorders, including depressive episodes, may include other features, such as: Anxious distress, when you're feeling symptoms of anxiety and fear that you're losing control. Melancholy, when you feel very sad and have a deep loss of pleasure. |
| Bipolar Disorder - National Institute of Mental Health (NIMH) | Bipolar I disorder is defined by manic episodes that last for at least 7 days (nearly every day for most of the day) or by manic symptoms that are so severe that the person needs immediate medical care. Usually, depressive episodes occur as well, typically lasting at least 2 weeks. |
| Bipolar Depression: Symptoms, Diagnosis, and Treatment - Healthline | Bipolar depression refers to the depressive episodes that are part of the mood cycling in bipolar disorder. Evidence shows that bipolar depressive episodes tend to last longer than... |
| Bipolar Depression Symptoms, Causes, and Treatment | This article explores the symptoms, causes, and diagnosis of bipolar depression, as well as some treatment and coping strategies that may be helpful. |
| Bipolar Disorder - Diagnosis and treatment - Mayo Clinic | This is true whether you're having a manic or major depressive episode. The main treatments for bipolar disorder include medicines and talk therapy, also known as psychotherapy, to control symptoms. Treatment also may include education and support groups. |
| Bipolar Disorder (Manic Depression): Symptoms & Treatment | Bipolar disorder is a chronic mood disorder that causes intense shifts in mood, energy levels and behavior. Manic and hypomanic episodes are the main sign of the condition, and most people with bipolar disorder also have depressive episodes. The condition is manageable with medications, talk therapy, lifestyle changes and other treatments. |
| 9 Treatments for Bipolar Disorder Depression - Healthline | From structuring your day to staying active, here are nine ways to boost your mood during a depressive episode. We’ll also provide an overview of what symptoms to look for. |
| Bipolar Stages: 3 Phases to Be Aware of - Healthline | Research Trusted Source shows that depressive episodes tend to be more severe (more frequent, longer-lasting, and disabling) in bipolar II than in bipolar I. Cyclothymic disorder:... |
| Bipolar Disorder: Symptoms, Causes, Types, and More - Psych Central | Many people with bipolar I disorder experience hypomanic and depressive episodes, too. Bipolar II disorder: Doctors diagnose bipolar II after at least one depressive episode and at least... |
| Bipolar Disorder: Symptoms, Causes, Treatment - WebMD | Bipolar disorder is a mental health condition that used to be called manic depression. If you have it, your moods can swing between periods of extreme... |